Understanding Electronic Medical Record Data
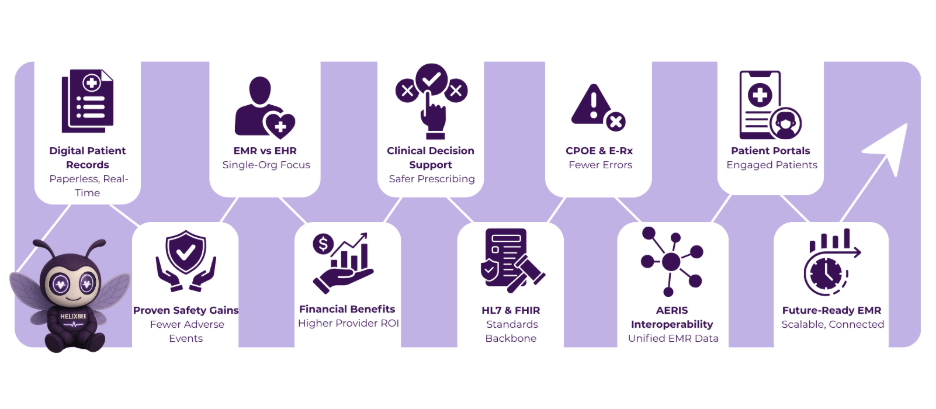
Electronic medical record data forms the backbone of modern healthcare delivery. This digital collection of patient information has replaced paper charts in most hospitals and clinics worldwide. Healthcare providers now rely on electronic medical record data to document patient encounters, track treatment plans, and support clinical decisions in real time.
What Is Electronic Medical Record Data?
Electronic medical record data refers to the digital version of a patient’s paper chart, but with far greater depth and accessibility. It includes medical history, medications, allergies, immunization records, laboratory results, radiology images, vital signs, personal demographics, billing information, and provider notes—all stored in a structured digital format within a single healthcare organization.
Unlike electronic health records (EHRs), which are designed to be shared across different healthcare organizations, electronic medical record data typically remains within one practice or hospital system. The distinction matters because electronic medical record data focuses on the treatment a patient receives from a specific provider, while EHR data follows the patient across multiple providers and settings.
Key Components of Electronic Medical Record Data
Electronic medical record data contains several standardized categories:
- Demographic information – name, date of birth, gender, address, contact details, insurance information
- Clinical documentation – progress notes, consultation reports, operative reports, discharge summaries
- Medication records – current and past prescriptions, allergies, adverse drug reactions
- Laboratory and pathology results – blood tests, microbiology cultures, biopsy reports
- Diagnostic imaging – X-rays, CT scans, MRIs, ultrasounds (often linked as DICOM files)
- Problem lists – active and resolved medical conditions using ICD-10 coding
- Immunization records – dates and types of vaccines administered
- Vital signs and measurements – blood pressure, heart rate, height, weight, BMI trends
- Orders and results – provider orders for tests, procedures, and consultations
These components are usually captured using standardized code sets such as SNOMED CT, LOINC, RxNorm, and ICD-10 to allow structured data entry and retrieval.
Benefits of Electronic Medical Record Data
Implementation of electronic medical record systems yields measurable gains:
1. Improved Patient Safety
Legible, complete, and instantly accessible records reduce medical errors caused by illegible handwriting or missing paper charts.
2. Better care coordination within a practice:
Every member of the care team can view the same up-to-date electronic medical record data, reducing duplicate testing and conflicting treatments.
3. Enhanced clinical decision making
Built-in clinical guidelines, drug interaction checkers, and population health analytics rely on high-quality electronic medical record data
4. Increased operational efficiency
Automated appointment reminders, e-prescribing, and electronic billing all stem from accurate electronic medical record data.
5. Research and public health reporting
De-identified electronic medical record data powers large-scale epidemiological studies and disease surveillance programs.
Challenges and Limitations
Despite the advantages, electronic medical record data presents several ongoing challenges:
- Data silos – Because most EMR systems are not designed for nationwide interoperability, electronic medical record data often remains trapped within a single institution.
- Data quality issues – Copy-paste practices, template overuse, and dropdown menu selections can introduce inaccuracies into electronic medical record data.
- Physician burnout – Excessive time spent entering electronic medical record data contributes to clinician fatigue and reduced patient interaction.
- Cybersecurity risks – High-profile ransomware attacks on hospitals have highlighted the vulnerability of centralized electronic medical record data repositories.
Standards and Interoperability Efforts
The healthcare industry has developed several standards to improve the usefulness of electronic medical record data:
- HL7 v2 and FHIR – messaging standards for exchanging clinical data
- Continuity of Care Document (CCD) – standardized XML format for summary records
- USCDI (United States Core Data for Interoperability) – defines a common set of data classes required for exchange
- 21st Century Cures Act – mandates information-blocking prohibitions and API access to electronic medical record data
AERIS: Streamlining Electronic Medical Record Systems Through FHIR Interoperability
AERIS, developed by Helixbeat, serves as an integration engine that connects disparate electronic medical record systems across US healthcare organizations. By leveraging HL7 and FHIR standards, AERIS normalizes data from multiple sources into a single, actionable view.
Ready to cut delays by 50%, double your ROI, and empower your team with instant access to critical data? Let’s dive into why AERIS is the solution you’ve been waiting for.
How AERIS Solves Core Challenges in Electronic Medical Record Systems
US providers rely on electronic medical record systems from different vendors. AERIS bridges these gaps without replacing existing EMR investments.
- Fragmented Data Flows – Legacy HL7 v2 interfaces require custom mapping for every endpoint.
- Delayed Transitions of Care – According to ONC 2023 data, fewer than half (42 %) of hospitals send summary‑of‑care records to most or all external hospitals and ambulatory providers, and only around 16‑17 % send them to most or all long‑term/post‑acute or behavioral health providers.
- High Integration Costs – Industry estimates suggest building an interoperable health app with HL7/FHIR integration can require $65,000–$130,000 in development costs; individual vendor interface packages (e.g., for major EHR systems) may start at $75,000 and go much higher.
AERIS automates these processes using FHIR APIs and USCDI v4 profiles.
Helixbeat by the Numbers
- 20+ Years of Expertise: Our team brings decades of healthcare IT experience to ensure AERIS works for you.
- 50+ IT Professionals: A dedicated crew powers AERIS, delivering unmatched support and innovation.
- 1,000+ Customers: Join a thriving community of healthcare leaders already transforming with AERIS.
- 10,000+ Projects Completed: Proven success across countless integrations and workflows.
- 95% Returning Customers: Our clients trust AERIS to deliver, time and time again.
The AERIS Advantage: Numbers That Speak for Themselves
Metric | Without AERIS | With AERIS | Your Benefit |
Data Exchange Delays | Frequent bottlenecks | Reduced by 50%
| Faster care in emergencies |
Return on Investment | Slow, costly overhauls | 100% faster ROI | Grow without breaking the bank |
Operational Costs | High redundancies | Cut by 30% | Save thousands annually |
Error Rates | Up to 20% manual errors | Slashed by 90% | Precision for better patient outcomes |
Your Benefits, Amplified
- 50% Fewer Delays: Real-time data means critical information is always at your fingertips, turning hours into seconds.
- 100% Faster ROI: Plug-and-play integration maximizes your investment without expensive system replacements.
- 30% Cost Savings, 90% Fewer Errors: Automation eliminates waste, saving resources and ensuring accuracy.
How AERIS Works: Your 3-Step Path to Success
- Connect Seamlessly: Integrate AERIS effortlessly into your existing systems, from legacy EMRs to modern platforms.
- Share Securely: Activate real-time data exchange with HIPAA-compliant encryption. Watch your teams and partners collaborate effortlessly.
- Optimize and Grow: Because AERIS evolves with your organization, it’s set up to help you succeed for the long haul.
What Users Say About AERIS
Dr. Sarah L.
Hospital Administrator
John T.
Telemedicine Provider
Emily P.
Healthcare Executive
FAQs
1.What standards support EMR interoperability?
Standards like HL7 v2, FHIR, Continuity of Care Document (CCD), USCDI, and policies from the 21st Century Cures Act help make EMR data more exchangeable and actionable.
2. Why is interoperability important for EMR data?
Interoperability allows healthcare systems to share and access patient information across platforms and organizations, turning EMR data into actionable insights for care and research.
3. How does AERIS help with EMR interoperability?
AERIS integrates disparate EMR systems using HL7 and FHIR standards, normalizing data from multiple sources into a single actionable view without replacing existing EMRs.
4. What problems can AERIS address in EMR systems?
AERIS reduces fragmented data flows, speeds up transitions of care, lowers integration costs, and minimizes manual errors by automating data exchange across systems.
Final Thoughts
Electronic medical record data has transformed healthcare delivery. However, the true power of EMR data lies in nationwide interoperability—the ability for healthcare systems to seamlessly share and access patient information across platforms, facilities, and geographies. Achieving this level of connectivity will enable EMR data to move from static documentation to an intelligent, actionable resource.
Ready to transform your EMR workflows and accelerate interoperability?


