Revenue Cycle Management (RCM) is the financial lifeline of any healthcare organization. Yet, many providers still rely on traditional RCM systems—think manual billing processes, siloed departments, legacy software, and fragmented communication. While these methods may have served well in the past, the evolving landscape calls for more agility, accuracy, and automation.
If you’re planning to move from a traditional RCM system to a more modern, tech-driven solution, you’re not alone. But transitions like these aren’t just plug-and-play—they require thoughtful planning, collaboration, and process adaptation.
Here are six practical tips to make the move from traditional RCM systems to modern revenue cycle technologies smoother and more rewarding.
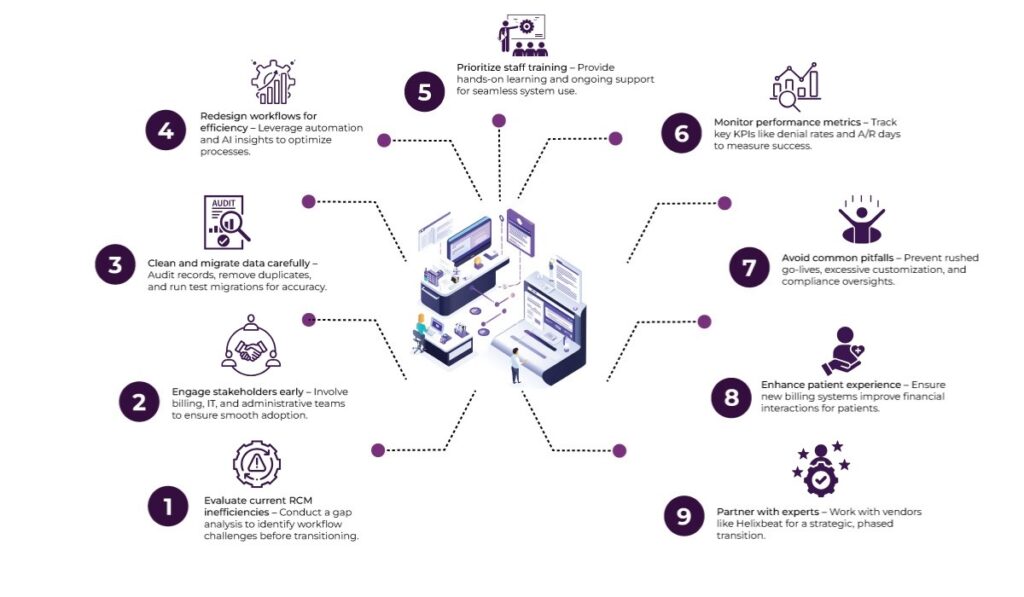
Table of Contents
1. Start With a Gap Analysis
Before diving headfirst into a new RCM platform, it’s important to understand what your current system does (and doesn’t do). A gap analysis will give you a clear picture of the existing workflows in your traditional RCM systems, their limitations, and opportunities for improvement.
Key Actions
- Map out each step in your current revenue cycle—from patient registration to final payment.
- Identify where delays, errors, or inefficiencies occur most frequently.
- Evaluate the performance of existing tools, such as your billing software or claim scrubbing engine.
Why it matters: Without a thorough audit, it’s easy to replicate old inefficiencies in a new system. By documenting your pain points and goals, you’ll lay the foundation for smarter decision-making and tech adoption.
2. Involve Your Team Early
Technology upgrades often fail not because the tools are flawed, but because the people using them aren’t brought into the process early. One of the biggest challenges with moving away from traditional RCM systems is resistance from front-desk teams, billers, coders, and even providers.
Key Actions
- Form a cross-functional transition team with representatives from billing, IT, clinical, and administrative departments.
- Conduct early-stage discussions to gather input and concerns.
- Offer visibility into how new systems will support individual roles and daily tasks.
Why it matters: When staff feel consulted and heard, they’re more likely to engage with new processes and adopt them successfully. Plus, they often bring valuable insights into real-world challenges the system needs to address.
3. Prioritize Data Migration and Clean-Up
Moving from traditional RCM systems to a new platform involves transporting large volumes of sensitive and historical data. Whether it’s patient demographics, billing histories, or claims data, a successful transition depends on the accuracy and completeness of the information.
Key Actions
- Perform a data audit to check for duplicate records, outdated information, and formatting inconsistencies.
- Collaborate with your new software vendor or integration partner to build a secure, compliant migration plan.
- Back up your old system and run test migrations before going live.
Why it matters: Clean data leads to cleaner claims and fewer rejections. Failing to prepare your data in advance could result in billing delays, revenue leaks, or compliance issues down the line.
4. Rethink and Redesign Workflows
Modern RCM platforms often come with automation, AI-powered insights, and real-time dashboards. However, these benefits can’t be fully realized if you try to mirror outdated processes within a new system. Therefore, transitioning from traditional RCM systems should be seen as a chance to reimagine how work gets done.
Key Actions
- Reevaluate manual tasks that could be automated, such as eligibility checks or claim status tracking.
- Use the implementation phase to redesign workflows for better speed and coordination.
- Align your workflows with new system capabilities, such as AI-based denial prediction or patient self-service portals.
Why it matters: A new RCM tool isn’t just about digitizing the old—it’s about transforming revenue cycle operations into something more predictive, efficient, and patient-friendly.
5. Invest in Training and Ongoing Support
The success of your transition depends heavily on how well your staff can navigate the new system. Unlike traditional RCM systems, modern platforms often involve a steep learning curve, especially for users unfamiliar with automation, analytics, or new coding protocols.
Key Actions
- Roll out hands-on training programs tailored to different user roles (front office, back office, clinical staff, etc.).
- Develop a resource library with training videos, cheat sheets, and FAQs.
- Set up a support structure for troubleshooting during the first few months post-implementation.
Why it matters: No matter how intuitive a system is, your team will need time and guidance to use it effectively. A well-trained team reduces errors, shortens the transition period, and accelerates ROI from your new investment.
6. Monitor KPIs Closely and Iterate
Your job isn’t done once the new system is live. In fact, the post-implementation phase is critical. To maximize the value of your transition, it’s vital to monitor revenue-related KPIs and make iterative improvements.
Key Actions
- Track metrics such as Days in A/R, first-pass resolution rate, denial rate, clean claim ratio, etc.
- Compare pre- and post-transition performance using historical benchmarks.
- Hold monthly review meetings to assess progress and optimize workflows.
Why it matters: Real-time performance monitoring helps you quickly spot what’s working and what isn’t. This iterative approach turns the transition into a continual improvement journey.
Common Pitfalls to Avoid During the Transition
While the six tips above help smooth the transition, knowing what not to do is just as important. Here are a few common mistakes that healthcare organizations face when leaving traditional RCM systems behind:
- Rushing the go-live date: Speed is good, but skipping thorough testing can cause chaos.
- Not accounting for compliance updates: Your new system must support current coding rules, data privacy laws, and payer mandates.
- Over-customizing the new system: Too much customization can create maintenance nightmares and complicate future upgrades.
- Ignoring patient experience: Billing is part of the patient journey. Upgraded RCM should also improve how patients interact with your office.
Avoiding these pitfalls can save time, money, and a lot of frustration during and after the transition process.
How Helixbeat Helps You Transition Smoothly from Traditional RCM Systems
Shifting from legacy Revenue Cycle Management (RCM) systems to a more advanced, integrated platform can be challenging—but Helixbeat makes it seamless and strategic.
To begin with, Helixbeat offers interoperability-ready infrastructure that connects with your existing EHRs, billing platforms, and third-party applications without forcing a complete overhaul. Instead of a disruptive replacement, the transition becomes a gradual transformation—one that aligns with your operational goals and timelines.
In addition, our support team works closely with your stakeholders—offering onboarding assistance, compliance guidance, and tailored configurations that align with your specific billing processes and payer mix. It’s not just about switching systems; it’s about building a better, more responsive RCM foundation for your future.
Do you want more insights on modernizing your RCM operations? Let’s discuss the tools and services that can move your healthcare revenue management into the future.
FAQs
1. Why should we move away from traditional RCM systems?
Traditional RCM systems often rely on manual workflows, outdated software, and siloed communication, leading to inefficiencies, delays, and errors. Modern systems offer better accuracy, automation, and integration.
2. What is a gap analysis, and why is it important during the RCM transition?
A gap analysis helps you assess what your current system is lacking and what improvements are needed. It prevents carrying over inefficiencies into the new platform.
3. What are common mistakes to avoid during RCM transitions?
Avoid rushing go-live, neglecting compliance requirements, over-customizing the system, and overlooking patient experience in billing workflows.
4. How much training is needed for staff on the new RCM platform?
Training should be role-specific and hands-on. Providing a resource library and dedicated support during the initial months can accelerate comfort with the system.
5. How can Helixbeat support our RCM system transition?
Helixbeat provides interoperability-ready infrastructure, tailored onboarding support, and close collaboration with your team to make the shift strategic and low-risk.













