Healthcare organizations today face a growing demand for operational efficiency, timely reimbursements, and reduced administrative burdens. Amidst rising labor costs, staff shortages, and increasingly complex payer policies, offshore revenue cycle management (RCM) services are becoming a practical and strategic solution.
Offshoring no longer carries the stigma it once did. In fact, many leading hospitals, physician groups, and medical billing companies are actively partnering with offshore RCM providers to improve their financial outcomes while focusing more on patient care.
Here are seven reasons why healthcare providers should seriously consider offshore revenue cycle management services.
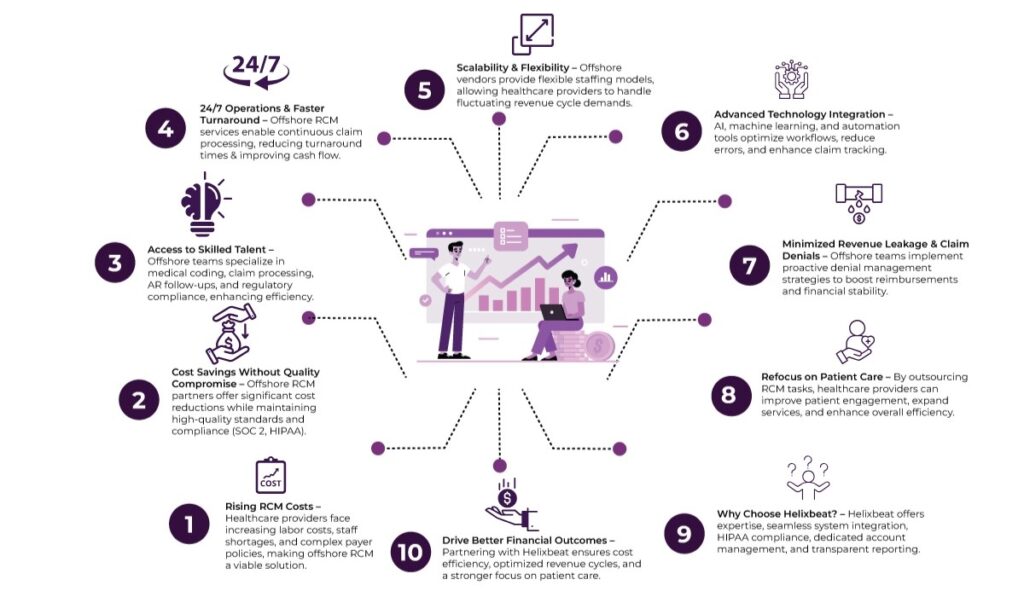
Table of Contents
1. Significant Cost Savings Without Compromising Quality
By partnering with RCM service providers, healthcare organizations can cut operational costs by streamlining processes, reducing administrative overhead, and improving billing efficiency.
But cost-effectiveness doesn’t mean lower quality. Most of these organizations also hold recognized certifications such as SOC 2, HIPAA, etc., reinforcing their commitment to data security and operational excellence. Therefore, RCM partners deliver a rare combination of cost efficiency, regulatory compliance, and consistent performance.
2. Access to Skilled and Specialized Talent
The RCM process isn’t just about billing. It involves complex workflows such as patient eligibility verification, medical coding, claim submission, AR follow-up, denial management, and reporting. Each of these steps requires a deep understanding of medical terminology, payer rules, and regulatory updates.
Offshore RCM providers typically have specialized teams trained in ICD-10 coding, CPT codes, Medicare and Medicaid policies, and private payer requirements. These professionals work in focused departments with dedicated quality control units, which boosts the efficiency of the entire revenue cycle.
With offshore staffing, healthcare providers gain access to a much larger talent pool that might not be readily available locally due to workforce shortages or budget limitations.
3. Round-the-clock operations and Faster Turnarounds
Offshore teams can operate during night hours and facilitate overnight claims, payments, and denial processing. This 24/7 capability drastically reduces turnaround times and accelerates cash flow.
For example, a claim entered into the system in the evening U.S. time can be processed and submitted to the payer by the time the office opens the next day. This continuous workflow is complex to replicate with in-house or domestic-only operations, especially when working within tight staffing budgets.
4. Scalability During High-Demand Periods
Revenue cycle volumes are rarely constant. Billing surges after holidays, flu seasons, or policy changes can quickly overwhelm in-house teams. Besides, hiring and training new staff for short-term spikes isn’t always feasible—and that’s where offshore RCM partners shine.
Offshore vendors offer flexible staffing models that scale up or down based on your volume. Whether you need 5 coders today and 15 next month, they can provide the resources without the administrative headaches of recruitment, onboarding, or training.
This elastic capacity allows providers to maintain continuity, handle backlogs efficiently, and avoid revenue leakage due to missed claims or deadlines.
5. Advanced Technology and Automation Tools
Many offshore RCM companies are early adopters of AI, machine learning, and robotic process automation (RPA) to improve workflow accuracy and reduce manual intervention. They often integrate their platforms with leading practice management systems (PMS) and electronic health record (EHR) software. These tools can automate repetitive tasks such as:
- Eligibility checks
- Claim status tracking
- Payment posting
- Denial code identification
With built-in dashboards and analytics, offshore RCM partners can offer real-time visibility into claim statuses, payment trends, and KPIs. This level of transparency allows providers to make data-driven decisions quickly.
6. Lower Risk of Revenue Leakage and Claim Denials
Revenue leakage is a silent killer. It happens due to undercoding, incorrect eligibility checks, missed filing deadlines, or claim denials that are never followed up on. Offshore RCM providers are hyper-focused on denial prevention and recovery, often implementing rigorous checks before a claim goes out. These providers:
- Audit claims before submission
- Track rejections in real-time
- Use historical data to predict and resolve common denial patterns
- Maintain SOPs for each payer requirement
Because their business model is performance-driven, they often have Service Level Agreements (SLAs) that commit to specific benchmarks like First Pass Resolution Rate (FPRR) or Days in Accounts Receivable (DAR). This proactive approach helps plug financial leaks and improves reimbursement rates.
7. Focus on Core Healthcare Services
Perhaps the most important reason of all: outsourcing RCM tasks allows your team to refocus on clinical care and patient satisfaction. Physicians and hospital staff are often burdened with administrative tasks, which affects both morale and productivity.
By delegating backend processes like medical billing, coding, and AR follow-up to an offshore team, providers can reclaim time and energy for:
- Improving patient engagement
- Expanding clinical services
- Innovating with telehealth or digital health tools
- Enhancing staff training and satisfaction
This shift from being bogged down in billing to operating at the top of their license leads to better healthcare outcomes and long-term organizational growth.
Why Choose Helixbeat as a Revenue Cycle Management Partner
Selecting the right medical revenue cycle management (RCM) partner can significantly impact your organization’s financial health and operational efficiency. Here’s why Helixbeat stands out:
1. Specialized Experience in Your Medical Field
Helixbeat covers ICD-10-CM, CPT, and HCPCS standards to minimize claim rejections and maximize reimbursements. With our team of certified coders and robust claim submission workflows, we help healthcare providers reduce delays, stay compliant, and improve cash flow from day one.
2. Proven Success with Similar-Sized Practices
Whether you’re a growing clinic or a large hospital network, Helixbeat has a proven track record of optimizing revenue cycles for healthcare providers of all sizes. Our case studies highlight real-world results, from improved collections to reduced denials.
3. Robust Data Security & HIPAA Compliance
Helixbeat adheres to the highest standards in data protection, including full HIPAA compliance, encrypted data exchange, and regular audits to keep your sensitive information safe.
4. Seamless Integration with EHR & PM Systems
Helixbeat offers seamless integration with leading EHR and Practice Management systems to minimize disruption and facilitate smoother workflows.
5. Dedicated Account Managers & Clear SLAs
With Helixbeat, every client is assigned a dedicated account manager who serves as a single point of contact—backed by service level agreements (SLAs) that clearly define response times, performance benchmarks, and accountability.
6. Transparent Reporting & Real-Time Dashboards
Helixbeat’s intuitive dashboards and transparent reporting provide real-time insights into collections, claims, denials, and key financial KPIs.
Final Thoughts
Offshore revenue cycle management services offer a compelling mix of cost efficiency, specialized talent, faster processing, and scalable support—making them a strategic choice for modern healthcare organizations. With access to advanced technology and a strong focus on revenue recovery, offshore RCM partners empower providers to streamline operations and prioritize patient care.
Looking for a trusted RCM partner?
Helixbeat brings deep industry expertise, cutting-edge automation tools, and a performance-driven approach to every client engagement. Whether you’re a solo practitioner or part of a multi-specialty group, we tailor our solutions to fit your needs and drive measurable results.
Contact us today and take the first step toward a more efficient, patient-focused, and profitable healthcare practice.
FAQs
1. Will offshoring compromise the quality of billing and coding services?
No. Most offshore RCM providers like Helixbeat are certified, follow global standards like HIPAA, SOC 2, etc., and have trained professionals to deliver high-quality, compliant services.
2. What types of tasks can be outsourced to offshore RCM providers?
Tasks include medical coding, patient eligibility verification, claim submission, AR follow-up, denial management, payment posting, and analytics reporting.
3. Can offshore RCM partners handle fluctuating workloads?
Yes. Offshore providers offer scalable staffing models that allow healthcare organizations to adapt to seasonal or volume-based changes quickly.
4. Is patient data safe with offshore RCM providers?
Reputable offshore providers follow strict data protection protocols, including encryption, compliance audits, and access controls aligned with HIPAA standards.
5. How does outsourcing RCM allow healthcare providers to focus on patients?
By offloading backend tasks, clinical staff can dedicate more time to patient care, service expansion, and other core healthcare functions.