The world of healthcare is constantly evolving, and keeping financial operations smooth is just as important as delivering quality patient care. Revenue cycle management (RCM) sits at the heart of this balance, shaping how providers handle billing, payments, and reimbursements.
However, with shifting regulations, emerging technologies, and rising patient expectations, healthcare organizations must adapt to stay ahead. These advancements are not just improving efficiency—they’re redefining how financial workflows operate. Let’s dive into the key trends reshaping healthcare billing and what they mean for the future.
Table of Contents
1. Shift Toward Value-Based Reimbursement Models
Traditional fee-for-service (FFS) models are gradually shifting to value-based reimbursement, where payments depend on patient outcomes rather than the volume of services provided.
Impact on RCM
- Rewards for High-Quality Care: Providers are now evaluated on patient recovery rates, reduced complications, and overall treatment effectiveness.
- Data-Driven Billing: Metrics like readmission rates, patient satisfaction, and recovery times become critical factors in payment determination.
- Managing Financial Risks: With reimbursements tied to performance, hospitals and clinics must navigate potential payment delays or penalties when benchmarks aren’t met.
Therefore, healthcare providers must integrate cutting-edge analytics and digital tools that help them refine billing strategies, monitor key performance indicators, and adapt to the evolving landscape of value-based care.
2. The Rise of Consumer-Driven Healthcare and Patient-Centric Billing
Patients today are more informed, financially conscious, and involved in their healthcare decisions than ever before. As a result, healthcare organizations must rethink their approach to patient billing and engagement.
Key Trends in Patient-Centric Billing
- Transparent Pricing: Patients want upfront cost estimates before receiving care, leading to greater demand for price transparency tools.
- Flexible Payment Options: Providers are offering installment plans, interest-free financing, and digital wallets to accommodate their financial situations.
- User-Friendly Billing Platforms: Healthcare billing is becoming more consumer-friendly, with intuitive online portals, mobile payment options, and real-time cost tracking.
By making the billing process more transparent and accessible, healthcare organizations can improve patient satisfaction while reducing payment delays and bad debt.
3. Increased Regulatory Compliance and Data Security Measures
As healthcare billing becomes more digitalized, organizations must navigate complex regulatory requirements to maintain compliance and protect sensitive patient data.
Evolving Compliance Challenges
- HIPAA and Data Protection: Stricter enforcement of patient privacy laws requires robust cybersecurity measures in billing and payment processing.
- No Surprises Act: New regulations are preventing unexpected medical bills by requiring clear cost communication between providers and patients.
- Interoperability Standards: As electronic health records (EHRs) and billing systems integrate, compliance with interoperability guidelines is necessary for smooth data exchange.
Therefore, healthcare organizations are investing in compliance training and secure digital platforms to protect patient information and meet regulatory standards.
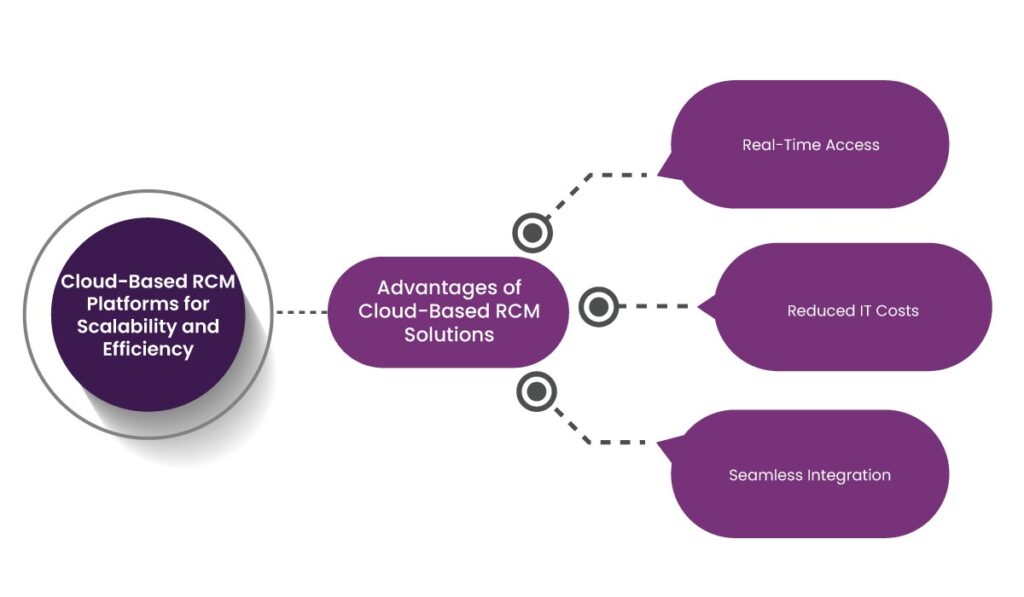
4. Cloud-Based RCM Platforms for Scalability and Efficiency
The adoption of cloud-based RCM solutions is accelerating as healthcare organizations seek scalable and cost-effective ways to manage their billing operations.
Advantages of Cloud-Based RCM Solutions
- Real-Time Access: Providers can access financial data and analytics from anywhere, facilitating better decision-making.
- Reduced IT Costs: Cloud platforms eliminate the need for expensive on-premise infrastructure, lowering operational expenses.
- Seamless Integration: Cloud-based systems easily connect with EHRs, practice management software, and payer networks, improving workflow efficiency.
By migrating to the cloud, healthcare organizations can streamline billing operations, reduce overhead costs, and enhance financial performance.
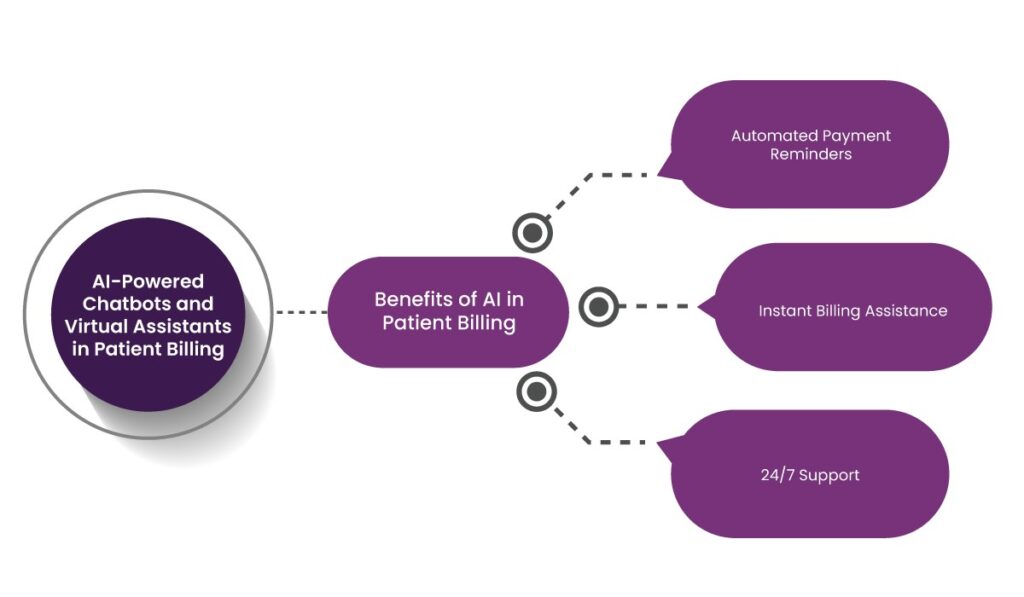
5. AI-Powered Chatbots and Virtual Assistants in Patient Billing
As patient interactions become increasingly digital, AI-driven chatbots and virtual assistants are playing a big role in revenue cycle management.
Benefits of AI in Patient Billing
- Automated Payment Reminders: AI can send personalized payment reminders, reducing instances of missed payments.
- Instant Billing Assistance: Patients can receive real-time answers to billing questions, improving engagement and satisfaction.
- 24/7 Support: Virtual assistants provide round-the-clock assistance and reduce the burden on human staff.
By incorporating AI into patient billing workflows, healthcare organizations can enhance efficiency, reduce administrative costs, and improve patient communication.
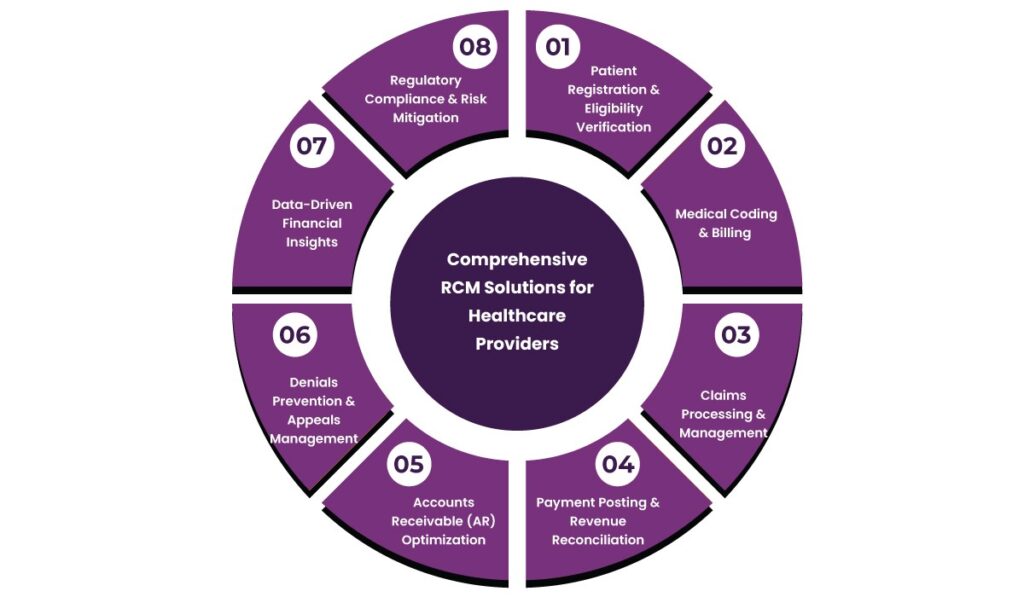
Why Partner with Helixbeat for Revenue Cycle Management?
Helixbeat delivers a robust Revenue Cycle Management (RCM) solution designed to optimize financial performance, minimize revenue leakage, and streamline operations for healthcare providers. Our end-to-end approach helps organizations navigate the complexities of medical billing, claims processing, and regulatory compliance with greater efficiency.
Comprehensive RCM Solutions for Healthcare Providers
1. Patient Registration & Eligibility Verification
Accurate data collection and real-time insurance verification prevent claim rejections by confirming patient eligibility at the start. This reduces the administrative burden and accelerates reimbursement timelines.
2. Medical Coding & Billing
Our certified coders apply precise ICD-10-CM, CPT, and HCPCS coding to maintain compliance while reducing errors. We handle claims submission, payment tracking, and billing accuracy, helping providers receive correct reimbursements without administrative delays.
3. Claims Processing & Management
From submission to resolution, we oversee the entire claims process. Our team proactively tracks pending claims, engages with payers, and applies strategic denial management techniques to recover lost revenue.
4. Payment Posting & Revenue Reconciliation
Every payment is meticulously recorded, with discrepancies instantly addressed to provide a transparent financial overview. This detailed tracking supports better revenue forecasting and financial planning.
5. Accounts Receivable (AR) Optimization
Aging claims can disrupt cash flow. Therefore, our AR specialists monitor outstanding payments, follow up on overdue balances, and implement workflows that accelerate revenue recovery.
6. Denials Prevention & Appeals Management
We analyze denial trends, identify root causes, and implement corrective measures to reduce future denials. As a result, our appeals management process strengthens claim approvals and enhances provider reimbursements.
7. Data-Driven Financial Insights
Helixbeat provides real-time dashboards and in-depth financial reports, helping providers monitor revenue trends, track claim statuses, and make informed business decisions.
8. Regulatory Compliance & Risk Mitigation
With a structured approach to compliance, we help providers stay aligned with HIPAA, payer contract requirements, and industry regulations. Our internal audits and controls reduce risk and safeguard financial integrity.
Final Thoughts
The rapid evolution of healthcare billing is reshaping how providers manage their revenue cycles. With the industry shifting toward value-based care, patient-centric billing, stringent regulatory requirements, and AI-driven automation, adapting to these changes is vital for financial stability and operational efficiency.
However, managing the intricacies of healthcare billing requires expertise, precision, and the right technology. That’s where Helixbeat help healthcare providers reduce claim denials, improve cash flow, and stay compliant with evolving regulations. If you’re ready to optimize your revenue cycle management, contact us today!
FAQs
1. How does value-based reimbursement impact healthcare billing?
Unlike traditional fee-for-service models, value-based reimbursement ties payments to patient outcomes, rewarding providers for delivering high-quality care rather than the volume of services provided.
2. Why is patient-centric billing becoming more important?
Patients are now more involved in their healthcare decisions and expect transparent pricing, flexible payment options, and user-friendly billing platforms that simplify the payment process.
3. How do cloud-based RCM platforms improve billing operations?
Cloud-based solutions provide real-time access to financial data, reduce IT infrastructure costs, and integrate seamlessly with EHRs and other healthcare systems for streamlined workflows.
4. What role does AI play in patient billing?
AI-powered chatbots and virtual assistants help automate payment reminders, provide instant billing support, and offer 24/7 assistance, improving efficiency and patient satisfaction.
5. What are the benefits of outsourcing RCM services?
Outsourcing RCM services helps healthcare providers reduce administrative burdens, speed up reimbursement processes, minimize revenue leakage, and stay compliant with evolving regulations.
6. How can Helixbeat help healthcare organizations optimize their revenue cycle?
Helixbeat offers end-to-end RCM solutions, including patient eligibility verification, claims management, denials prevention, financial analytics, and regulatory compliance, helping providers streamline billing operations and improve revenue collection.