Healthcare is rapidly evolving, not just in terms of patient care and clinical innovation, but also in how providers manage their financial operations. One major shift behind the scenes is the increasing adoption of outsourced medical billing and revenue cycle management. Today, hospitals, clinics, and even solo practitioners are looking beyond in-house teams and embracing external partners to handle the journey from patient registration to final payment.
This growing reliance on medical revenue cycle management services is a strategic move in times of rising administrative costs, tighter margins, and a complicated insurance landscape. So, why is this shift happening now, and what are the real pros and cons? Let’s dive into the benefits, challenges, and outlook of outsourcing this critical function.
Table of Contents
What is Medical Revenue Cycle Management?
Before exploring why providers are outsourcing it, let’s clarify what medical revenue cycle management (RCM) involves. RCM covers everything from verifying patient insurance and coding diagnoses to submitting claims, processing denials, collecting payments, and generating financial reports.
In short, medical revenue cycle management services help healthcare providers get paid for the care they deliver—accurately, efficiently, and on time.
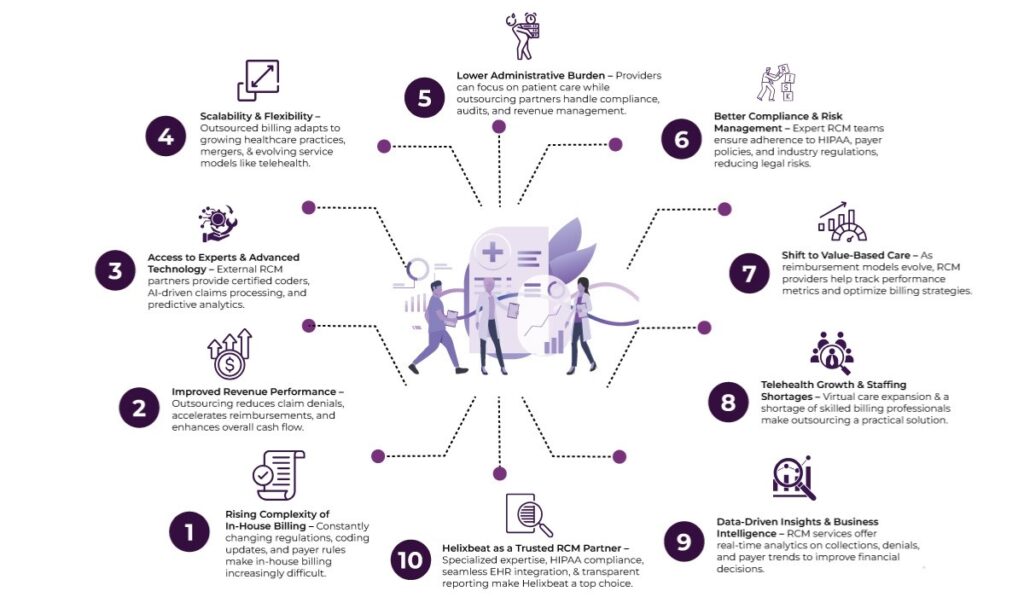
The Rising Complexity of In-House Billing
The healthcare payment system is anything but straightforward. With constantly changing payer rules, new regulations like the No Surprises Act, evolving ICD and CPT coding guidelines, and value-based care models gaining traction, billing is no longer a task for a general administrative team.
Many practices struggle with:
- Claim denials due to coding errors or incomplete documentation
- Delayed reimbursements
- Lack of transparency in collections and performance analytics
- Staff shortages and high turnover in billing departments
These challenges often result in lost revenue, poor cash flow, and staff burnout. That’s where outsourced medical revenue cycle management services step in—offering expertise, scalability, and tech-driven solutions.
Top Benefits of Outsourcing Medical Billing and RCM
1. Improved Revenue Performance
Perhaps the most compelling reason healthcare providers are outsourcing is the measurable improvement in collections. Third-party billing companies optimize claim submissions, reduce denials, and accelerate reimbursements. Their teams are trained to handle complex billing scenarios across various specialties and payer contracts.
Therefore, providers can increase their cash flow and invest more in patient care and operations by minimizing errors and maximizing revenue opportunities.
2. Access to Trained Experts and Advanced Technology
RCM vendors live and breathe healthcare finance. They stay updated with the latest billing codes, payer policies, and compliance mandates. When a provider partners with them, they gain access to a dedicated team of certified coders, auditors, analysts, and billing specialists—all without the hassle of hiring and training in-house staff.
Many RCM service providers also bring cutting-edge tools like AI-driven claims scrubbing, predictive analytics, and cloud-based dashboards, which can streamline operations and offer actionable insights.
3. Scalability and Flexibility
As healthcare businesses grow, so do their billing needs. Outsourcing offers the flexibility to scale operations up or down without disrupting workflows. Whether it’s a multispecialty hospital or a niche telehealth provider, medical revenue cycle management services can adapt to different volumes and specialties seamlessly.
This agility is especially valuable during rapid expansion, mergers, or transitions in EHR and practice management systems.
4. Lower Administrative Burden
Running an in-house billing team requires constant attention—from hiring and training to managing software, compliance checks, and audits. For many providers, these administrative duties pull focus away from patient care.
By outsourcing, healthcare providers can redirect internal resources toward core clinical activities while the billing partner takes care of backend processes.
5. Better Compliance and Risk Management
Billing errors don’t just lead to lost income—they can trigger audits, fines, and reputational damage. Outsourced RCM partners have dedicated compliance teams to navigate state and federal regulations, payer rules, and industry standards like HIPAA.
Their structured approach to documentation, auditing, and denial management helps reduce risk and maintain clean records.
Key Trends Driving the Outsourcing Boom
So why is this surge in outsourcing happening now? Here are some macro trends pushing healthcare organizations toward external RCM support:
1. Shift to Value-Based Care
As the industry moves from fee-for-service to value-based care, billing becomes more outcome-driven and data-intensive. Outsourced RCM partners can help track metrics, align coding with care quality, and handle risk-sharing models with greater ease.
2. Rise of Telehealth and Virtual Care
The pandemic accelerated the growth of telehealth, which brought new challenges in coding, documentation, and payer reimbursement. Many virtual care startups and hybrid practices lack the internal bandwidth to handle complex billing, making outsourcing a practical choice.
3. Shortage of Skilled Healthcare Workers
Billing and coding professionals are in short supply, particularly in smaller towns and rural areas. Outsourcing solves the talent gap by providing access to qualified specialists without geographic constraints.
4. Healthcare Consolidation and M&A Activity
As healthcare systems merge and expand, billing systems become more fragmented. Outsourcing RCM helps standardize processes across locations, integrate revenue streams, and reduce redundancies.
5. Focus on Analytics and Business Intelligence
Today, medical revenue cycle management services don’t just submit claims—they generate insights. Providers want more visibility into payer behavior, denial patterns, reimbursement timelines, and patient payment trends. RCM partners equipped with advanced analytics tools are stepping up to meet this demand.
Why Choose Helixbeat as a Medical Revenue Cycle Management Partner
Selecting the right medical revenue cycle management (RCM) partner can significantly impact your organization’s financial health and operational efficiency. Here’s why Helixbeat stands out:
1. Specialized Experience in Your Medical Field
Helixbeat covers ICD-10-CM, CPT, and HCPCS standards to minimize claim rejections and maximize reimbursements. With our team of certified coders and robust claim submission workflows, we help healthcare providers reduce delays, stay compliant, and improve cash flow from day one.
2. Proven Success with Similar-Sized Practices
Whether you’re a growing clinic or a large hospital network, Helixbeat has a proven track record of optimizing revenue cycles for healthcare providers of all sizes. Our case studies highlight real-world results, from improved collections to reduced denials.
3. Robust Data Security & HIPAA Compliance
Helixbeat adheres to the highest standards in data protection, including full HIPAA compliance, encrypted data exchange, and regular audits to keep your sensitive information safe.
4. Seamless Integration with EHR & PM Systems
Helixbeat offers seamless integration with leading EHR and Practice Management systems to minimize disruption and facilitate smoother workflows.
5. Dedicated Account Managers & Clear SLAs
With Helixbeat, every client is assigned a dedicated account manager who serves as a single point of contact—backed by service level agreements (SLAs) that clearly define response times, performance benchmarks, and accountability.
6. Transparent Reporting & Real-Time Dashboards
Helixbeat’s intuitive dashboards and transparent reporting provide real-time insights into collections, claims, denials, and key financial KPIs.
Final Thoughts
With rising complexities in billing regulations, increasing administrative pressures, and a stronger push toward data-driven care, more healthcare providers are recognizing the long-term value of working with expert RCM partners.
That’s where Helixbeat comes in. Whether you run a small clinic, a specialty practice, or a multi-location hospital network, Helixbeat offers scalable, secure, and insight-driven revenue cycle management solutions designed to help your business thrive. From expert coding and billing to powerful analytics and dedicated account support—Helixbeat helps healthcare organizations unlock operational clarity and consistent cash flow.
Partner with Helixbeat today and take the first step toward smarter revenue cycle management.
FAQs
1. What are medical revenue cycle management services?
Medical revenue cycle management services involve managing the entire financial process of a healthcare provider—from patient registration and insurance verification to medical coding, claims submission, denial management, and payment collections.
2. Why are healthcare providers outsourcing medical revenue cycle management services?
Providers are outsourcing these services to improve cash flow, reduce administrative burdens, access skilled professionals, and stay compliant with evolving regulations, all while focusing more on patient care.
3. Can medical revenue cycle management services integrate with my current EHR system?
Yes, leading RCM providers like Helixbeat offer seamless integration with most EHR and practice management systems, allowing smoother data exchange and workflow continuity.
4. What should I look for in a provider of medical revenue cycle management services?
Key factors include specialty expertise, proven success with similar practices, strong data security, integration capabilities, flexible pricing, and dedicated account support—qualities you’ll find with Helixbeat.