Mergers in the healthcare industry sound promising—improved patient care, reduced operational costs, and broader reach. But for anyone who’s been through one, you know it’s not all smooth sailing. One of the biggest headaches? Data incompatibility. When two hospitals or health systems merge, they often use different Electronic Health Record (EHR) systems. That’s where chaos begins. Imagine trying to align two entirely different patient record formats, different coding systems, and distinct workflows—all while maintaining HIPAA compliance and patient safety.
And the worst part? This isn’t a one-time issue. Every new partnership can reignite the same data drama. That’s why Fusion’s FHIR implementation in healthcare is becoming a game-changer. With a well-structured FHIR server, organizations can bridge data silos, enable smooth EHR integration in mergers, and support real-time interoperability in healthcare.
In this blog, we’ll break down how Fusion’s FHIR for data sharing works, why it matters in mergers, and how it tackles your real-world data problems.
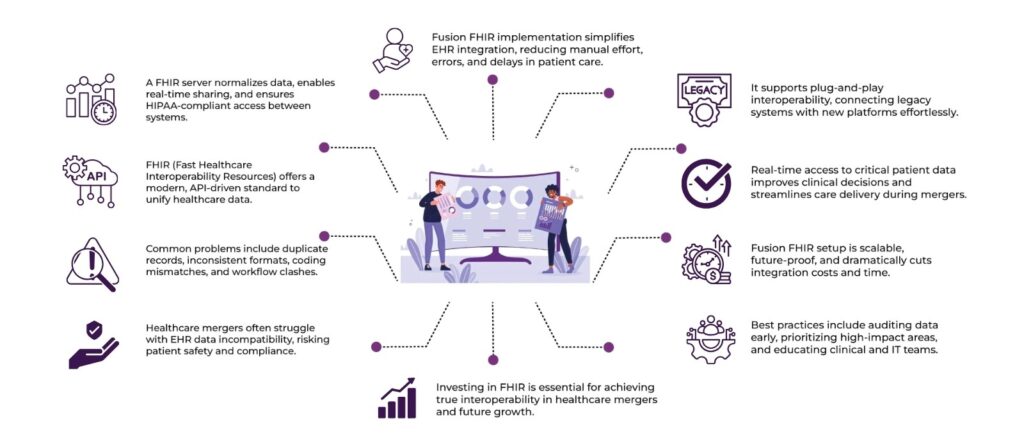
Table of Contents
The Messy Reality of Healthcare Mergers
Let’s say Hospital A and Hospital B decide to merge. Their vision? Unified care. Their reality? Systems that refuse to talk to each other. Hospital A uses Epic. Hospital B uses Cerner. The IT teams are pulling all-nighters just to get patient histories, medication lists, and imaging data to sync.
Here’s what typically goes wrong:
- Duplicate records due to incompatible formats.
- Lost or inaccessible patient data.
- Delays in care due to manual data entry.
- Compliance issues with data security protocols.
That’s not just inefficient—it’s dangerous. When patient records aren’t accurate or accessible in real-time, it can lead to medical errors. This is exactly why FHIR implementation in healthcare has taken center stage.
Common Data Incompatibilities in Healthcare Mergers
Here are the common types of data incompatibilities that occur:
1. Different Data Formats
- One system might store dates as DD-MM-YYYY, another as MM/DD/YYYY.
- One EHR might use XML, another JSON, or even flat files (CSV, TXT).
- Lab results, diagnoses, or images may be stored and structured differently.
2. Varying Data Models and Schemas
- Hospital A might store patient allergies under one field, while Hospital B has it split across multiple fields.
- Medication lists might be structured differently: one may separate dosage, route, and frequency, while the other bundles them together.
- One EHR might allow free text for “diagnosis,” while another requires structured ICD-10 codes.
3. Inconsistent Terminologies and Coding Standards
- Different use of medical vocabularies like ICD-10, SNOMED CT, LOINC, or CPT.
- One system might refer to “Myocardial Infarction,” another as “Heart Attack,” and another by ICD-10 code “I21.”
- This makes matching or comparing data extremely difficult without standardization.
4. Data Access and Security Protocols
- Different authorization/authentication mechanisms (OAuth, SAML, etc.).
- Some systems may encrypt data differently or limit API access to specific endpoints.
- During a merger, these differences block smooth data flow or even full access.
5. Duplicate or Incomplete Records
- A single patient might be listed multiple times across systems under different IDs.
- Demographic information (e.g., name, address, phone) may be outdated or missing in one system but current in another.
- Merging records without introducing errors becomes difficult.
6. Workflow Incompatibilities
- Some data is created or updated based on workflows unique to a specific system.
- For instance, lab orders, radiology reports, or discharge summaries might be triggered differently, resulting in missing or mismatched data during integration.
7. Lack of Interoperable Interfaces
- Legacy systems may not have APIs or web services at all.
- Others might have proprietary APIs that don’t conform to open standards like FHIR.
- This makes real-time communication and integration very hard.
8. Time Zone and Locale Issues
- Systems across regions might store timestamps in different formats or time zones.
- Medication timings, appointment records, or treatment durations might get misaligned if not normalized.
9. Patient Matching Errors
- If two systems don’t follow the same identifiers or master patient index (MPI), it can lead to:
- Mismatched patients
- Missing records
- Privacy issues
These incompatibilities don’t just slow down the merger process—they can have real clinical consequences: duplicated tests, misdiagnosis, delayed treatment, or in the worst case, patient harm.
This is exactly why FHIR implementation in healthcare is such a critical solution. FHIR standardizes data, offers APIs for integration, and helps unify different systems under one interoperable framework
What is FHIR, and Why Is It a Big Deal?
FHIR implementation in healthcare is a data standard developed by HL7 to simplify the exchange of healthcare information across systems. But what makes it different from older standards like HL7 v2 or CDA?
It’s modern, modular, and API-friendly—think of it as the “Spotify of FHIR for data sharing” compared to the “cassette tape” of old-school EHR systems.
Here’s what makes FHIR implementation in healthcare awesome:
- It uses web standards like REST, JSON, and XML.
- It allows developers to create lightweight APIs for easy integration.
- It’s extensible, so it adapts to your organization’s unique data needs.
- It enables real-time access to patient data across different platforms.
So, when it comes to EHR integration in mergers, FHIR implementation in healthcare eliminates much of the manual rework that bogs teams down.
FHIR Servers: The Backbone of Integration
A FHIR server is like the interpreter in a multilingual meeting. It stores healthcare data in FHIR format and enables systems to exchange that data effortlessly, regardless of their original architecture.
During a merger, when you’ve got different EHRs trying to “talk,” a FHIR server becomes the central hub. It translates and shares data between systems using standardized FHIR resources (like Patient, Observation, AllergyIntolerance, etc.).
Key Features of a FHIR Server:
- Data normalization: It brings all incoming data into a common format.
- APIs for sharing: It lets EHRs fetch or send data through secure, RESTful APIs.
- Scalability: Whether you’re integrating two clinics or ten hospitals, it scales easily.
- Security & Compliance: Built-in access control ensures HIPAA compliance.
Without a FHIR server, FHIR implementation in healthcare can’t deliver its full potential. With it, you can rapidly achieve interoperability in healthcare—which, let’s face it, is the holy grail in mergers.
How Fusion FHIR Implementation in Healthcare Solves Data Compatibility Issues
When healthcare organizations merge, one of the toughest roadblocks is the incompatibility of their data. This is where Fusion FHIR implementation in healthcare becomes a true game-changer. Fusion FHIR (Fast Healthcare Interoperability Resources) acts like a universal translator—it ensures that all data, regardless of format or origin, can be seamlessly understood and shared between systems.
1. Standardised Data Format
Fusion FHIR uses a common data format and structure, which eliminates the typical chaos caused by different EHR systems using their own custom formats. With FHIR, patient data, lab reports, billing info, and more are structured in a unified way—making EHR integration in mergers much more streamlined.
2. Plug-and-Play Interoperability
Think of Fusion FHIR as a smart adapter that allows old legacy systems to communicate with modern platforms. This plug-and-play model supports rapid interoperability in healthcare, helping newly merged organizations avoid the painful process of completely replacing existing systems.
3. Real-Time Access to Critical Data
During a merger, delays in accessing patient history, prescriptions, or lab results can disrupt care. Fusion FHIR for data sharing across systems, ensuring clinicians have immediate access to the information they need. This reduces duplicate tests and improves patient outcomes.
4. Simplifies Integration Workflows
Traditional data integration involves complex ETL (Extract, Transform, Load) processes. Fusion FHIR drastically simplifies this with APIs designed specifically for healthcare, reducing time, effort, and cost for IT teams working on EHR integration in mergers.
5. Reduces Data Loss & Errors
When data is manually transferred or reformatted, it’s vulnerable to errors. FHIR’s structured format ensures that sensitive information like allergies, medication, or diagnoses is transmitted with accuracy, protecting patient safety during and after the merger.
6. Scalability for Future Systems
FHIR isn’t just about current integration—it sets up the organisation for the future. Fusion FHIR implementation in healthcare ensures that as new systems are added or updated, they can easily connect without requiring the entire integration process to be repeated from scratch.
Best Practices for FHIR Implementation in healthcare During Mergers
- Start with a data audit: Know what systems you’re dealing with and identify data overlaps.
- Choose the right FHIR server: Look for scalability, compliance features, and vendor support.
- Focus on high-impact use cases first: Prioritize patient history, medications, and allergies.
- Educate your teams: Clinicians and IT teams need to understand how FHIR workflows impact their daily work.
- Measure impact continuously: Track improvements in data access, clinical outcomes, and operational efficiency.
A successful FHIR implementation in healthcare isn’t just about the tech—it’s about aligning people, processes, and platforms.
Final Thoughts: FHIR is the Future of Connected Care
Healthcare mergers will continue. So will the challenge of merging data. But with FHIR, we have a framework that makes it possible—and even seamless—to bring systems together. A FHIR for data sharing acts as the glue, offering real-time, standardized, and secure access to health data across organizations.
By investing in FHIR implementation in healthcare, organizations can stop fearing mergers and start embracing them—with less disruption, better patient care, and long-term digital health success.
So if your organization is heading toward a merger—or just planning for the future—start with Fusion. It’s not just a tech upgrade. It’s your ticket to real interoperability in healthcare.
FAQs
Q1: How is FHIR helping the healthcare industry?
FHIR is revolutionizing healthcare by enabling seamless data exchange between different systems, improving care coordination, and supporting real-time access to patient information.
Q2: Why is FHIR useful?
FHIR is useful because it standardizes healthcare data, supports RESTful APIs, and enables interoperability across different EHR systems with minimal development effort.
Q3: What are some FHIR resources required for exchanging data?
Common FHIR resources include:
Patient (patient demographics)
Observation (lab results)
AllergyIntolerance (allergy records)
MedicationRequest (prescriptions)
Encounter (visit details)
Condition (diagnoses)
Q4: What are the benefits of FHIR for healthcare?
FHIR improves data accuracy, accelerates information exchange, lowers integration costs, enhances patient safety, and future-proofs systems with scalable architecture.
Q5: What are the challenges to using FHIR for healthcare interoperability?
Challenges include varying EHR implementations, inconsistent data quality, lack of skilled developers, integration with legacy systems, and ensuring data security compliance.
Q6: What are some challenges to using aggregated and intelligently applied data to solve aspects of the healthcare system?
Key challenges are data silos, lack of standardization, privacy concerns, and difficulty in deriving actionable insights from complex or unstructured data.
Q7: What challenges can be solved using data in the healthcare sector?
Data can help solve issues like delayed diagnoses, care gaps, duplicate testing, medication errors, resource mismanagement, and population health tracking.