Today, the healthcare sector has made incredible strides in technology and innovation, yet it faces a glaring challenge—data fragmentation. In an era where industries thrive on interconnected systems, healthcare continues to grapple with silos, inefficiencies, and a lack of communication between systems.
In this blog, we’ll explore the challenges of fragmented healthcare systems, the growing necessity for seamless data exchange, and why interoperability in healthcare is critical for providers.
Table of Contents
The Promise and Peril of Healthcare Data
By 2025, the volume of healthcare data is expected to skyrocket, with a projected compound annual growth rate of 36%. From electronic health records (EHRs) to wearable health trackers, the potential for leveraging this information to improve patient outcomes is immense. However, this explosion of data comes with its own set of challenges:
1. Data Fragmentation
Patient information often resides in disparate systems maintained by hospitals, diagnostic labs, pharmacies, and insurance companies. These systems rarely communicate with each other, which creates ‘data silos.’ Therefore, healthcare providers struggle to see the complete picture of a patient’s health without a centralized or connected repository.
2. Inconsistent Standards
Different healthcare providers and technology platforms often use varied formats to store and transmit information. One hospital’s EHR system might record blood pressure readings in one format, while another uses an entirely different structure. Additionally, insurance companies, diagnostic labs, and telemedicine platforms add their formats to the mix, thus creating a labyrinth of incompatible systems.
Therefore, healthcare systems must focus on real-time data integration and streamlined workflows to mitigate these delays. By doing so, providers can act quickly and accurately, which enhances the quality of care.

The Cost of Fragmentation
Data silos in healthcare come with a steep price—both human and financial. A West Health Institute and the Global Healthcare Interoperability Market study estimates that lack of interoperability costs the US healthcare system over $30 billion annually. Beyond the monetary impact, fragmented data can have life-altering consequences:
1. Medication Errors
When healthcare providers lack access to a patient’s complete medication history, they’re nearly working blindfolded. For example, imagine a patient visiting a hospital with unexplained symptoms. The attending physician, unaware of the patient’s allergy to a particular antibiotic, prescribes medication that triggers a severe reaction. Such instances occur far too often without a unified healthcare system.
2. Duplicate Testing
Think about the frustration of re-taking a test you aced simply because the results were lost. Now imagine this happening in healthcare, where patients undergo blood tests, X-rays, or MRIs multiple times, not because of medical necessity, but due to a lack of communication between providers. This isn’t just inconvenient; it’s expensive, time-consuming, and, in some cases, physically taxing for patients.
3. Delayed Diagnosis
In healthcare, time isn’t just money—it’s life. Imagine a scenario where a patient arrives at the emergency room with symptoms of a stroke. The clock is ticking, but critical details about their medical history—like past conditions, current medications, or allergies—are scattered across multiple systems. As the medical team scrambles to piece together the puzzle, precious minutes slip away, and the risk of permanent damage or death increases. Therefore, delayed diagnoses can have catastrophic consequences, especially in critical care situations like strokes.
Therefore, it’s crucial to break down these data silos and create a more interconnected healthcare system.
What Is Interoperability in Healthcare?
Interoperability in healthcare refers to the ability of different healthcare systems, applications, and devices to communicate, exchange, and interpret data accurately and meaningfully. It operates on four levels:
- Foundational: Basic data exchange between systems without interpreting the content.
- Structural: Data exchange that follows standardized formats to maintain consistency.
- Semantic: Systems interpret exchanged data in a meaningful way and enable decision-making.
- Organizational: Governance and policy frameworks that support seamless data sharing across entities.
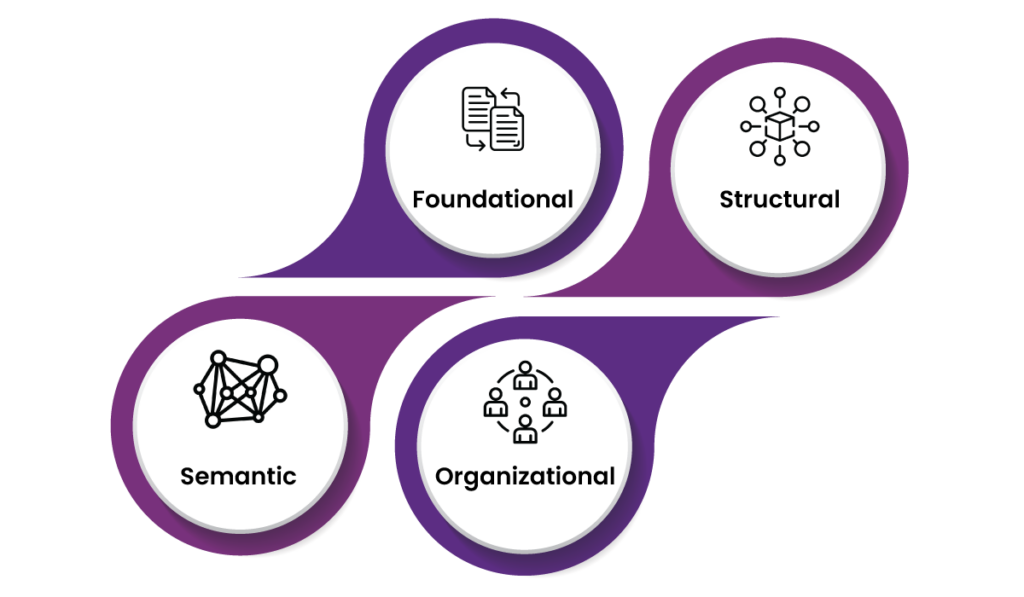
Achieving full interoperability in healthcare means breaking down technical, semantic, and organizational barriers to create a unified healthcare ecosystem.
Why Interoperability in Healthcare Is Non-Negotiable
Interoperability in healthcare is not just a technical requirement; it’s a cornerstone of value-based care. Here’s why it’s indispensable:
1. Improved Patient Outcomes
When healthcare providers have access to comprehensive patient data, they can make informed decisions faster. For example, a patient arriving in the emergency room with chest pain benefits greatly if the attending physician can instantly access their allergies, chronic conditions, and recent treatments.
2. Streamlined Care Coordination
Chronic disease management often involves multiple specialists and care teams. However, EHR interoperability bridges these communication gaps and facilitates a cohesive approach to treatment. For example, a diabetic patient’s endocrinologist, cardiologist, and primary care physician can collaborate effectively with shared access to lab results and medication regimens.
3. Reduced Costs
By minimizing duplicate tests and administrative inefficiencies, interoperability significantly cuts healthcare costs. A McKinsey report highlights that advanced data-sharing frameworks could save the global healthcare system $500 billion annually.
4. Enhanced Patient Experience
Patients increasingly expect digital, seamless interactions with their healthcare providers. Interoperability facilitates online appointment scheduling, telemedicine consultations, and easy access to personal health records, thus improving satisfaction and engagement.

Steps Toward Achieving Interoperability
Here’s a closer look at the critical steps needed to break down the barriers to seamless healthcare data exchange:
1. Adopt Universal Standards
Think of healthcare systems as people speaking different languages. Therefore, it’s nearly impossible to communicate without a shared vocabulary. However, universal standards like HL7 FHIR (Fast Healthcare Interoperability Resources) act as the Rosetta Stone for healthcare data. By adopting these standards, systems can exchange data easily. When providers can “speak” this universal language, it eliminates unnecessary delays, reduces manual data entry errors, and enhances patient care.
2. Emphasize Patient-Centric Solutions
At the heart of interoperability is the patient. Therefore, systems should be designed to prioritize ease of use, not just for healthcare professionals but also for patients. When patients have seamless access to their own health data, they become empowered participants in their care journey.
Imagine a digital platform where patients can view their medical history, lab results, and prescriptions in one place, regardless of which provider they visited. Such systems reduce frustration, simplify appointment management, and enhance trust in the healthcare system. However, this accessibility must be balanced with stringent safeguards to protect patient privacy and data security.
3. Encourage Innovation Through Open APIs
Open APIs (Application Programming Interfaces) help third-party developers to create innovative tools without being locked into a specific ecosystem. This adaptability can enhance patient care and streamline operations. For example, a fitness app can share wearable data with an EHR system with APIs. As a result, healthcare providers can gain better insights for personalized treatment.
Final Thoughts
By addressing the challenges of data silos and facilitating seamless data exchange, healthcare can unlock its true potential—delivering better outcomes, reducing costs, and empowering patients like never before.
Interoperability in healthcare isn’t just about technology; it’s about creating a connected ecosystem where information flows freely. In this connected future, patients won’t have to carry the burden of fragmented records, providers will work with confidence, and public health will thrive. It’s a vision worth striving for—a vision where interoperability is not negotiable but foundational.
FAQs
1. What is interoperability in healthcare?
Interoperability in healthcare refers to the ability of different applications, systems, and devices to exchange, interpret, and use data effectively.
2. Why is data fragmentation a significant issue in healthcare?
Data fragmentation occurs when patient information is stored in disconnected systems, which prevents healthcare providers from accessing comprehensive medical histories. Therefore, it leads to inefficiencies and delays in care.
3. What are the levels of interoperability in healthcare?
Healthcare interoperability operates on four levels:
- Foundational: Basic data exchange without content interpretation.
- Structural: Consistent formats for data exchange.
- Semantic: Meaningful data exchange to support decision-making.
- Organizational: Governance and policies for seamless data sharing.
4. How can universal standards like HL7 FHIR benefit healthcare systems?
Universal standards like HL7 FHIR enable consistent data formats, which makes it easier for disparate systems to communicate. This reduces errors, enhances data accuracy, and supports real-time information sharing.
5. What are the consequences of data silos in healthcare?
Data silos can result in medication errors, duplicate testing, and delayed diagnosis. These issues affect patient safety and place financial and operational burdens on healthcare systems.