In the age of advanced medical technology and digital transformation, one might assume that healthcare providers have seamless access to patient information. Yet, the reality is far from perfect. Fragmentation in healthcare data—the scattered, siloed, and uncoordinated nature of patient information—remains a persistent challenge. This disjointedness isn’t just a technological inconvenience; it carries significant costs that ripple through the healthcare ecosystem.
From financial burdens to compromised patient outcomes, fragmentation in healthcare data is a silent disruptor that needs addressing. In this blog, we’ll explore the multifaceted costs associated with fragmented healthcare data and discuss how it affects patients, providers, and the broader healthcare system.
Table of Contents
Financial Impacts of Fragmented Healthcare Data
Healthcare organizations spend billions annually attempting to reconcile fragmented data systems. A study by the West Health Institute estimates that the U.S. healthcare system could save over $30 billion annually by improving medical device interoperability, which would reduce redundant testing and manual data entry.
Moreover, the lack of integrated data systems contributes to medical errors, which are costly both in human and financial terms. The Institute of Medicine (IOM) estimates that medical errors incur an annual cost of $17 to $29 billion. In the U.S., a widely cited 2016 study by Johns Hopkins identified medical errors as the third leading cause of death, accounting for over 250,000 fatalities each year, with some estimates exceeding 400,000.
Impact on Patient Safety and Outcomes
Fragmentation in healthcare data isn’t just a financial burden—it can also jeopardize patient safety. When providers lack access to a complete and unified medical history, critical errors can occur, including:
1. Medication Errors
Doctors rely on comprehensive patient data to make informed decisions, but if crucial information—like allergies, previous adverse reactions, or existing medications—is missing, the risk of harmful drug interactions multiplies. For example, prescribing blood thinners without knowing a patient is already on another anticoagulant could lead to excessive bleeding.
2. Delayed Diagnoses
In chronic or progressive conditions, time is of the essence. The longer it takes to confirm a diagnosis, the more a condition can progress and narrow the window for effective intervention. For example, a patient who has undergone imaging for a suspicious growth might visit a specialist only to find the scans are unavailable due to system incompatibility. This delay could mean precious time lost in initiating potentially life-saving treatment.
3. Inconsistent Care Plans
Patients with chronic conditions, such as diabetes or rheumatoid arthritis, often require input from multiple specialists—endocrinologists, rheumatologists, cardiologists, and more. Each specialist may have their own approach, but without a shared platform to view the patient’s complete health history, care plans can conflict and even cause harm.

Operational Challenges for Providers
Let’s see how fragmentation in healthcare data complicates operational challenges:
1. Lengthy Data Retrieval
Instead of focusing on treatment strategies, healthcare staff spend precious time tracking down these records. The fragmented nature of data systems often means navigating through outdated software, contacting other facilities, or manually piecing together information from disparate sources. This inefficiency is frustrating and potentially harmful for healthcare teams operating under tight schedules.
2. Burnout Among Clinicians
Healthcare professionals, beyond their primary duties of diagnosing and treating patients, are now bogged down by tasks such as updating multiple databases, cross-checking records, and reconciling conflicting patient information. A study published in the Annals of Family Medicine by the American Medical Association and the University of Wisconsin revealed that physicians spend nearly six hours daily interacting with electronic health records (EHRs), both during and after clinic hours. This constant juggling directly contributes to rising stress levels and burnout among healthcare providers.
3. Reduced Collaboration
Modern healthcare thrives on interdisciplinary collaboration. For example, in oncology care, radiologists, oncologists, surgeons, and nurses must work in harmony to craft personalized treatment plans for patients. However, fragmentation in healthcare data systems creates silos and limits the ability of team members to access and share crucial patient information in real-time. Such obstacles can lead to incomplete treatment plans, miscommunications, or delays in initiating life-saving procedures.

How Can We Move Toward Data Integration
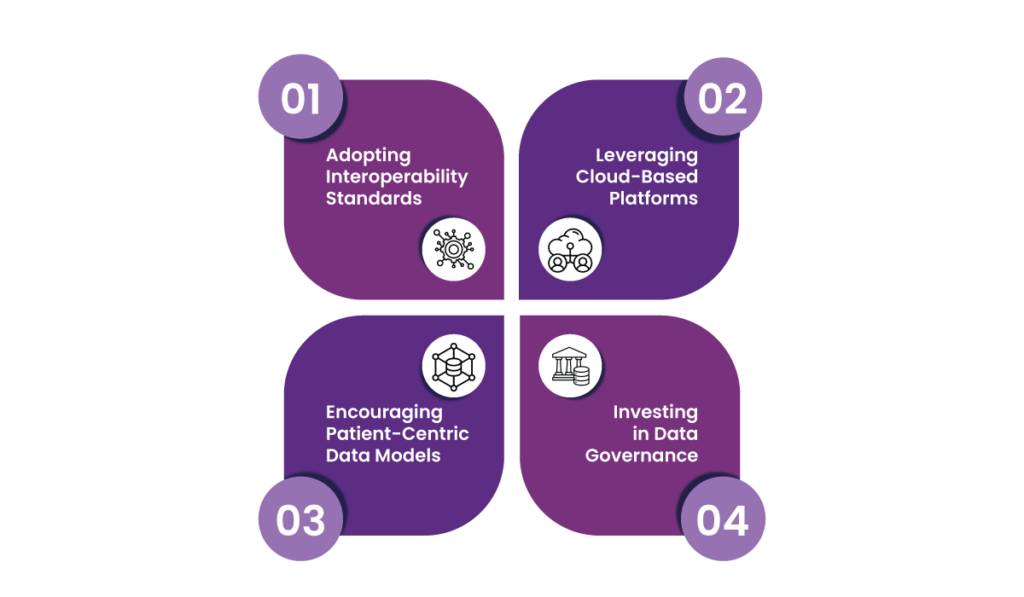
While fragmentation in healthcare data is a stubborn challenge, solutions exist to bridge these gaps. Here are some strategies:
1. Adopting Interoperability Standards
Interoperability standards like FHIR (Fast Healthcare Interoperability Resources) provide a common framework for different healthcare systems to communicate and share data. For example, when a patient moves from one provider to another, interoperability allows their medical history to follow them digitally. Beyond convenience, this holistic view helps providers make informed decisions quickly and reduce diagnostic errors.
2. Leveraging Cloud-Based Platforms
Cloud computing has revolutionized industries, and healthcare is no exception. By storing health data on the cloud, providers can access real-time information from virtually anywhere—be it in a hospital, a clinic, or even during a house call.
Take telemedicine, for example. Cloud-based platforms allow physicians to consult patients remotely with access to their health records, diagnostic reports, and even imaging files. This flexibility boosts collaboration among healthcare professionals and speeds up decision-making processes.
3. Encouraging Patient-Centric Data Models
What if patients became the custodians of their own health data? Patient-centric data models aim to make this vision a reality. By leveraging apps, digital wallets, or patient portals, individuals can store, access, and share their health records with providers as needed.
Imagine a scenario where a patient traveling abroad experiences a medical emergency. With a digital health wallet, they can instantly share critical medical history with the attending physician. This approach also promotes greater patient engagement and accountability, as they have direct control over their health information.
4. Investing in Data Governance
While integrating data is vital, maintaining its quality, security, and accessibility is equally important. This is where robust data governance comes into play. Therefore, organizations must establish clear protocols for collecting, storing, and accessing data.
For example, standardized data entry processes can minimize errors while stringent security measures protect sensitive patient information from breaches. Over time, effective governance builds trust among patients and providers, laying the groundwork for a more transparent and efficient healthcare ecosystem.
The Role of Technology in Driving Change
Emerging technologies are playing a pivotal role in addressing fragmentation in healthcare data:
- Artificial Intelligence (AI): AI can identify patterns in disparate datasets, improving diagnostics and care recommendations.
- Blockchain: Blockchain technology offers a secure way to share patient data while maintaining privacy.
- IoT Devices: Wearables and remote monitoring tools generate real-time data that can integrate with electronic health records (EHRs).

These innovations represent a step toward a more connected and efficient healthcare system.
The Bottom Line
Fragmentation in healthcare data is a costly issue—financially, operationally, and emotionally. Therefore, addressing this challenge requires a concerted effort to integrate data systems, adopt interoperability standards, and leverage advanced technologies.
The benefits of a unified data ecosystem go beyond cost savings. It enhances patient safety, improves outcomes, and creates a healthcare experience that inspires trust and confidence. By prioritizing data integration, the healthcare industry can move closer to delivering the seamless, high-quality care that every patient deserves.
FAQs
1. What is fragmentation in healthcare data?
Fragmentation in healthcare data refers to patient information scattered across different systems, which makes it difficult for providers to access a unified and complete medical history.
2. How does fragmented data impact healthcare costs?
Fragmentation in healthcare data leads to redundant tests, increased administrative burdens, and medical errors, resulting in billions of dollars in additional costs annually.
3. How do cloud-based platforms address data fragmentation?
Cloud-based platforms provide real-time access to patient records from anywhere, facilitating better collaboration and decision-making among healthcare professionals.
4. What technologies are helping to solve data fragmentation in healthcare?
Technologies like artificial intelligence (AI), blockchain, and IoT devices are used to integrate, secure, and analyze healthcare data for better outcomes.
5. What are the benefits of adopting interoperability standards like FHIR?
Standards like FHIR create a common framework for data sharing. This allows seamless transitions between providers and improves diagnostic accuracy.
6. How does fragmented healthcare data affect collaboration among providers?
Fragmentation in healthcare data creates silos, which limits the ability of interdisciplinary teams to access real-time patient information and create personalized treatment plans.














