The present healthcare landscape generates patient data at multiple points—whether from general practitioners, specialists, labs, pharmacies, or wearable devices. However, this rich trail of medical data often remains fragmented, leaving both patients and providers grappling with inefficiencies, repeated tests, or even delayed diagnoses.
This is where healthcare interoperability platform come into play. These platforms don’t just bridge data silos—they place the patient at the center of the care experience. By facilitating seamless information exchange, interoperability software transforms healthcare delivery, improves outcomes, and creates a smoother, more connected journey for every patient.

Table of Contents
The Shift Toward Patient-Centered Care
Patient-centered care is a healthcare philosophy that puts the patient’s needs, values, and experiences first. It means listening to the patient, personalizing treatment, and promoting transparency. But to make this approach practical, providers need access to comprehensive, up-to-date patient data.
This is where a robust healthcare interoperability platform becomes foundational. With it, providers can deliver coordinated care that feels more like a guided path. For example:
- A primary care physician can access a patient’s imaging results from a specialist
- A diabetic patient’s blood sugar readings from a wearable device can sync with their medical record
- Hospital discharge summaries can reach community caregivers instantly
These seamless handoffs reduce patient burden, minimize medical errors, and foster trust between patients and healthcare providers.
Real-Life Scenario: A Better Experience Through Interoperability
Let’s walk through the journey of a hypothetical patient named Anna.
Anna, a 58-year-old with hypertension and Type 2 diabetes, visits her primary care doctor after feeling lightheaded. Her doctor orders labs and refers her to a cardiologist. Traditionally, Anna might need to carry physical copies of her records or wait days for information to transfer.
But with a healthcare interoperability platform in place:
- Her lab results are automatically shared with both her primary doctor and cardiologist
- Her cardiologist reviews her history, prescribes medication, and updates the shared record
- The new prescription is instantly available at Anna’s local pharmacy
- Later, her primary doctor checks the cardiologist’s notes and follows up accordingly
All these touchpoints are connected, eliminating friction and confusion. More importantly, Anna feels heard, guided, and supported—key ingredients for a positive health outcome.
Enhancing Outcomes with Real-Time Data Exchange
Beyond convenience, interoperability drives better clinical outcomes. Here’s how:
1. Faster Diagnoses and Fewer Errors
Time matters in healthcare. With real-time access to test results, imaging data, and patient history, clinicians can make quicker, more informed decisions. This reduces the risk of medication interactions, misdiagnoses, or redundant tests.
2. Proactive Chronic Care Management
Chronic diseases like asthma, diabetes, and heart failure require ongoing monitoring. A healthcare interoperability platform can help providers track changes, spot trends, and intervene early, often before a condition worsens.
3. Smoother Care Transitions
When patients move between hospitals, rehabilitation centers, or home care settings, clear communication between providers is important. Interoperability supports smooth transitions, reducing hospital readmissions and improving recovery.
4. Empowered Patients
Interoperability also gives patients more control over their health journey. When individuals can access their records, test results, and care plans through digital platforms, they’re more likely to engage with their care and follow medical advice.
Key Features of an Effective Healthcare Interoperability Platform
Not all interoperability solutions are created equal. A platform that truly centers the patient should include:
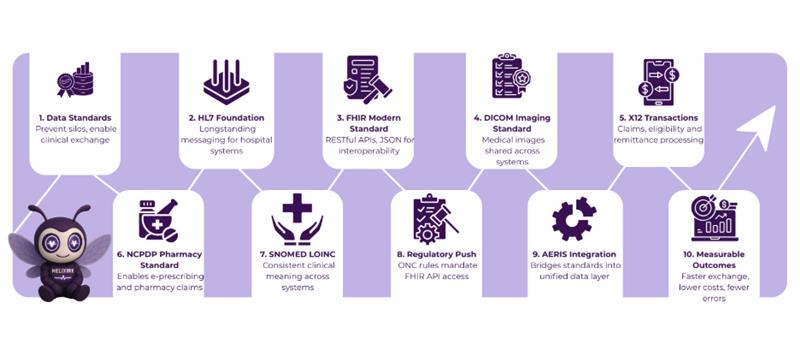
1. HL7 and FHIR Compliance
These are the leading data exchange standards that facilitate structured, secure data transfer across systems. FHIR (Fast Healthcare Interoperability Resources) in particular supports modern web-based data sharing, mobile apps, and wearable integrations.
2. Bidirectional Data Flow
Data shouldn’t just flow in one direction. A reliable platform should allow both sending and receiving of information in real time between systems, providers, and even patients.
3. Data Normalization and Mapping
Different systems use different data formats. A good interoperability platform converts and aligns data so it’s meaningful and usable across the ecosystem.
4. Security and Consent Management
Patients must feel confident that their data is protected. Interoperability software should offer advanced authentication, encryption, and consent frameworks that meet regional data privacy regulations like HIPAA.
5. Scalable Integration Capabilities
Whether connecting a small clinic or a national hospital network, the platform should scale easily, integrating with existing EHRs, lab systems, pharmacy tools, and more.
Interoperability and the Rise of Virtual Care
The global push for telemedicine and virtual care has made interoperability even more essential. Virtual consultations, remote diagnostics, and home monitoring all generate valuable data, but without a central bridge, much of this information gets lost.
A healthcare interoperability platform supports virtual care by:
- Aggregating real-time data from wearable devices
- Syncing virtual consults with in-person visits
- Allowing specialists to collaborate across cities or countries
- Facilitating e-prescriptions and remote follow-ups
This level of integration ensures that patients receive the same quality of care remotely as they would in a clinic, without gaps or delays.
Unlock Seamless Healthcare Interoperability with AERIS
AERIS is a cutting-edge healthcare interoperability platform designed to streamline data exchange across diverse healthcare systems. Whether it’s electronic health records (EHR), lab results, imaging systems, or third-party applications, AERIS makes critical patient data flow seamlessly, securely, and in real-time.
- Real-Time Data Exchange: AERIS makes patient data instantly available to healthcare providers, cutting down delays and speeding up decisions.
- FHIR and HL7 Compliance: Built with the latest data standards, AERIS supports FHIR (Fast Healthcare Interoperability Resources) and HL7 protocols, enabling smooth communication between systems.
- Enhanced Security and Compliance: AERIS is designed with patient privacy in mind, offering advanced encryption, authentication, and full compliance with healthcare regulations like HIPAA.
- Scalability for Healthcare Networks: Whether you’re a small clinic or a large hospital network, AERIS scales to meet the needs of any healthcare provider.
Final Thoughts
The promise of interoperability goes beyond technology—it’s about transforming the healthcare experience into something more humane, coordinated, and empowering. A healthcare interoperability platform is a critical foundation for this shift.
In a world where healthcare systems are often fragmented, AERIS is the solution that connects the dots, putting the patient at the center of care. Contact us to learn more about how AERIS can streamline your organization’s data management and create a connected, patient-first experience.
FAQs
1. How does a healthcare interoperability platform improve patient care?
By providing real-time access to patient data from multiple sources, a healthcare interoperability platform enhances communication among healthcare providers. This results in quicker diagnoses, more accurate treatment plans, and fewer errors.
2. What are the benefits of using a healthcare interoperability platform?
A healthcare interoperability platform offers numerous benefits, including:
- Streamlined data exchange between different healthcare systems
- Reduced duplication of tests and procedures
- Improved patient outcomes through better coordination
- Cost savings due to more efficient workflows
- Enhanced patient satisfaction with quicker, more coordinated care
3. Can a healthcare interoperability platform integrate with existing EHR systems?
Yes, a healthcare interoperability platform like AERIS is designed to integrate seamlessly with existing electronic health record (EHR) systems. It can connect various types of healthcare software, creating a unified data ecosystem that allows for better collaboration between providers.
4. Is a healthcare interoperability platform scalable for large healthcare networks?
AERIS is highly scalable, making it suitable for healthcare organizations of all sizes. Whether you’re a small clinic or a large hospital network, the platform can expand to meet your needs.