The financial health of healthcare organizations hinges on effective RCM. From patient registration and insurance verification to billing and payment collection, RCM covers every financial touchpoint in the patient care journey. However, as the landscape grows more complicated, many providers find themselves overwhelmed by rising administrative costs, compliance burdens, and staffing challenges. That’s where healthcare RCM outsourcing enters the picture.
But outsourcing RCM is a strategic decision. So, how do you know if your organization is ready to make the leap?
In this blog, we’ll explore what healthcare RCM outsourcing means, its potential benefits, and, most importantly, the key indicators that suggest your organization is ready for this move.
Table of Contents
What Is Healthcare RCM Outsourcing?
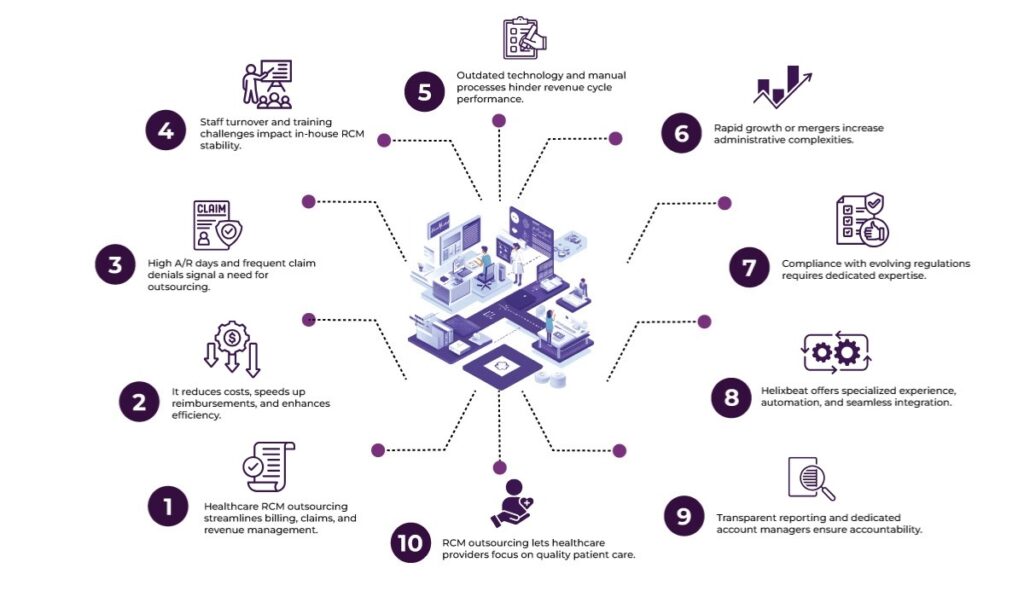
Healthcare RCM outsourcing involves delegating all or part of the revenue cycle processes to a third-party service provider. These companies specialize in handling administrative functions such as medical billing, claims management, denial resolution, coding, and accounts receivable (A/R) follow-up.
Instead of managing an in-house billing team, healthcare organizations rely on these experts to streamline operations, reduce claim denials, and speed up reimbursements. The goal? To improve financial outcomes while letting healthcare professionals focus on delivering quality care.
Why Consider Healthcare RCM Outsourcing?
Before we dive into the checklist, it’s worth looking at why healthcare providers — from small clinics to large hospital systems — are turning to RCM partners:
- Cost Efficiency: Outsourcing often reduces operational expenses by eliminating full-time billing staff, office space, and ongoing training costs.
- Access to Expertise: RCM firms bring deep industry knowledge, certified coders, and up-to-date tools that can handle frequent changes in payer rules or government regulations.
- Scalability: As patient volumes fluctuate, outsourced teams can scale their services accordingly — no need to hire or downsize staff continually.
- Faster Payments: Improved coding accuracy, denial management, and follow-up processes often translate into quicker reimbursements.
- Reduced Administrative Burden: Physicians and internal staff can focus on core clinical and patient-centric activities instead of chasing unpaid claims.
Signs Your Healthcare Organization Is Ready for RCM Outsourcing
Now comes the big question: How do you know if your healthcare organization is ready for healthcare RCM outsourcing? Below are key signs and situations to evaluate.
1. Your A/R Days Are Climbing
Accounts Receivable (A/R) days — the average time it takes to collect payment after rendering a service — is one of the most telling indicators of revenue cycle health. If your A/R days consistently exceed industry benchmarks (typically 30–40 days), it may be time to reassess.
Long A/R cycles often indicate inefficient billing practices, undertrained staff, or inadequate follow-up. An outsourced RCM provider brings structured workflows and dedicated teams to help shrink this timeline and improve cash flow.
2. You’re Dealing with High Staff Turnover
Billing and coding departments are notoriously high-stress areas, and retaining experienced RCM staff is no easy feat. Also, constant hiring, onboarding, and training of new staff drains time and resources.
If you’ve noticed a pattern of staff burnout or difficulty retaining billers and coders, healthcare RCM outsourcing could stabilize your operations. Outsourcing partners already have trained personnel who are ready to hit the ground running.
3. Coding Errors and Denials Are Affecting Revenue
Even minor coding mistakes can lead to claim rejections or denials, which directly impact reimbursement rates. If your denial rate exceeds 5–10%, you may be leaving a significant amount of money on the table.
Outsourced RCM firms typically employ certified coders who stay updated with the latest ICD-10, CPT, and HCPCS changes. They use automation and quality checks to identify and correct errors before claims are submitted, which reduces denials and boosts first-pass acceptance rates.
4. Technology Gaps Are Holding You Back
Modern revenue cycle processes rely heavily on digital tools — electronic health records (EHRs), billing platforms, clearinghouses, and analytics dashboards. If your organization struggles with outdated systems, manual processes, or lack of integration, it might be time to partner with a provider that brings advanced tech to the table.
RCM outsourcing partners often offer AI-enabled denial prediction, robotic process automation (RPA), real-time performance tracking, and EHR integrations — giving your team better visibility and control without investing heavily in new infrastructure.
5. You’re Expanding (or Merging) Rapidly
Growth is a good thing — but it can wreak havoc on your internal processes. Whether you’re opening new clinics, merging with another provider, or scaling services, the administrative load increases quickly.
Outsourcing gives you the flexibility to manage that growth without hiring an entirely new back-office team. The RCM partner can adapt quickly to your changing needs, align with new payer contracts, and onboard new providers into the billing system efficiently.
6. Compliance and Audit Risks Are Growing
Healthcare regulations change frequently — from HIPAA to payer-specific documentation rules. Staying compliant while also managing routine billing functions is a full-time job.
Outsourcing partners typically have dedicated compliance teams that conduct regular audits, keep track of regulation updates, and maintain detailed documentation trails. This helps minimize legal and financial exposure during payer audits or regulatory reviews.
Why Choose Helixbeat as a Healthcare RCM Outsourcing Partner
So, you’ve identified that your organization might be ready. But choosing the right partner is critical to success. Here’s why Helixbeat stands out:
1. Specialized Experience in Your Medical Field
Helixbeat covers ICD-10-CM, CPT, and HCPCS standards to minimize claim rejections and maximize reimbursements. With our team of certified coders and robust claim submission workflows, we help healthcare providers reduce delays, stay compliant, and improve cash flow from day one.
2. Proven Success with Similar-Sized Practices
Whether you’re a growing clinic or a large hospital network, Helixbeat has a proven track record of optimizing revenue cycles for healthcare providers of all sizes. Our case studies highlight real-world results, from improved collections to reduced denials.
3. Robust Data Security & HIPAA Compliance
Helixbeat adheres to the highest standards in data protection, including full HIPAA compliance, encrypted data exchange, and regular audits to keep your sensitive information safe.
4. Seamless Integration with EHR & PM Systems
Helixbeat offers seamless integration with leading EHR and Practice Management systems to minimize disruption and facilitate smoother workflows.
5. Dedicated Account Managers & Clear SLAs
With Helixbeat, every client is assigned a dedicated account manager who serves as a single point of contact—backed by service level agreements (SLAs) that clearly define response times, performance benchmarks, and accountability.
6. Transparent Reporting & Real-Time Dashboards
Helixbeat’s intuitive dashboards and transparent reporting provide real-time insights into collections, claims, denials, and key financial KPIs.
Final Thoughts
Healthcare RCM outsourcing isn’t just about cutting costs; it’s about creating the bandwidth for your organization to focus on what matters most: delivering exceptional patient care. Helixbeat brings industry-leading expertise, cutting-edge technology, and a personalized approach to revenue cycle management. Whether you’re navigating growth, compliance, or operational inefficiencies, we help transform your back office into a strategic powerhouse.
Contact us today to discover how our solutions can drive better outcomes.
FAQs
1. What is healthcare RCM outsourcing?
Healthcare RCM outsourcing involves assigning revenue cycle tasks—like billing, coding, and claims management—to a third-party provider. This helps streamline operations and improve payment timelines.
2. How can I tell if my organization is ready for healthcare RCM outsourcing?
Key indicators include rising A/R days, frequent coding errors, high staff turnover, outdated systems, compliance risks, or upcoming expansions or mergers.
3. Can outsourcing help reduce claim denials?
Yes. RCM outsourcing partners like Helixbeat use certified coders and advanced tools to catch errors early, resulting in fewer rejections and higher first-pass acceptance rates.
4. How does RCM outsourcing support regulatory compliance?
Yes, Helixbeat stays updated with healthcare regulations and conducts regular audits to help your organization stay aligned with HIPAA and payer-specific rules.
5. Will outsourcing disrupt my current EHR or PM system?
Not necessarily. Providers like Helixbeat offer seamless integration with existing EHR and practice management systems to maintain workflow continuity.