In healthcare, submitting medical claims accurately isn’t just about getting paid—it’s about keeping the system moving efficiently, maintaining trust with patients, and reducing administrative headaches. Yet, many healthcare providers still struggle with claim rejections, denials, and payment delays due to simple but costly errors.
Effective medical claims management begins with accurate claims submission. It saves time, boosts revenue, and strengthens relationships with both payers and patients. But how can providers get better at it? Let’s break it down with practical insights and strategies.
Table of Contents
The High Stakes of Claims Submission Accuracy
In the United States alone, it’s estimated that nearly 20% of all medical claims are denied or delayed due to errors. These issues cost providers billions each year, not to mention the time and labor involved in reworking the claims. The root cause? Often, it’s avoidable mistakes—incorrect patient information, mismatched codes, missing documentation, or billing the wrong payer.
An effective medical claims management system is key to navigating these challenges. When accuracy is prioritized, providers can cut down on denials, shorten revenue cycles, and create a more seamless patient experience.
Let’s explore how healthcare providers can significantly improve claims submission accuracy.
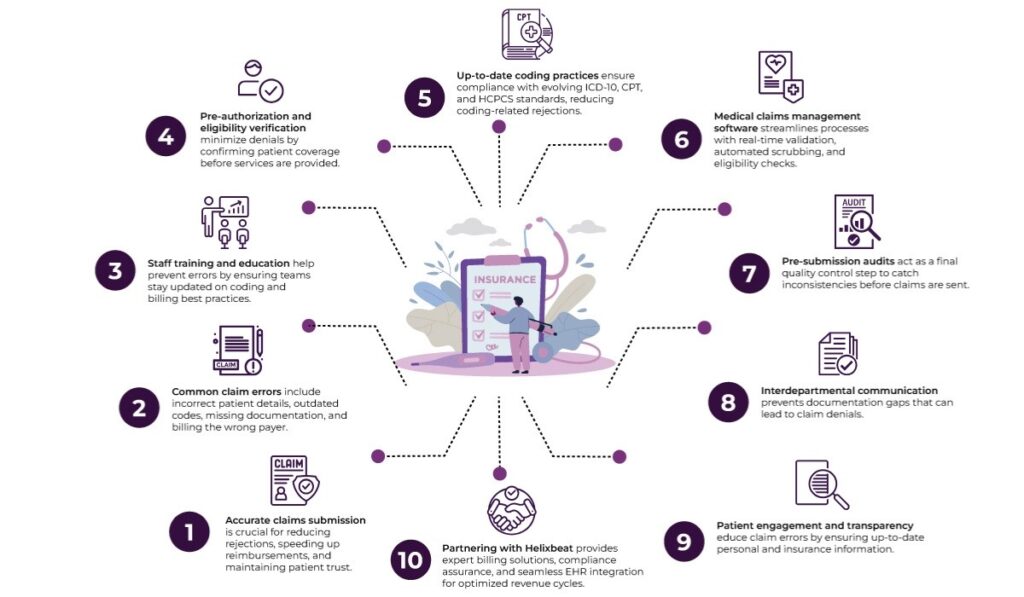
1. Invest in Staff Training and Education
Your front-line staff—those handling patient intake, coding, and billing—play a pivotal role in claims accuracy. If they don’t have the right training, errors are bound to creep in.
Why it matters: Incorrect patient demographics or insurance details at the registration stage can render even the most perfectly coded claim useless.
What you can do
- Offer regular training on evolving insurance policies and payer rules.
- Educate staff on common billing and coding errors.
- Encourage open communication between coding teams, physicians, and billing departments.
A well-trained team is the foundation of successful medical claims management.
2. Implement Robust Pre-Authorization and Eligibility Verification
Submitting claims without verifying patient eligibility or obtaining prior authorization is one of the fastest ways to get denied. These steps often get skipped due to time constraints, but the long-term cost is far greater.
What helps
- Use automated tools to verify insurance coverage before the visit.
- Confirm policy numbers, deductibles, co-pays, and any referral requirements.
- Document all pre-authorization reference numbers properly.
Making this process routine can drastically improve submission accuracy and reduce claim bounce-backs.
3. Adopt Standardized and Up-to-Date Coding Practices
Medical codes evolve constantly, and payers update their policies to reflect these changes. Whether it’s ICD-10, CPT, or HCPCS codes, using outdated or mismatched codes leads to immediate denials.
How to stay on track
- Use certified medical coders or outsource to professionals who stay current with industry changes.
- Subscribe to code update alerts from CMS or payer organizations.
- Use EHRs and billing software that auto-populate the latest code sets.
Accurate coding not only helps in faster claim processing but also prevents under- or overbilling, supporting ethical medical claims management practices.
4. Leverage Integrated Medical Claims Management Software
Modern billing tools are designed to reduce manual entry errors, flag missing information, and verify claims before submission. A good medical claims management platform can serve as a real-time quality control checkpoint.
Key features to look for
- Automatic code validation
- Real-time eligibility checks
- Pre-submission claim scrubbing
- Integrated clearinghouse functionalities
Software that integrates seamlessly with EHR and practice management systems eliminates redundancy and provides a centralized view of claim statuses.
5. Conduct Pre-Submission Claims Audits
Before hitting “submit,” a second pair of eyes (even if digital) can make a world of difference. Internal audits help spot inconsistencies and omissions that would otherwise lead to denials.
Effective audit practices
- Use claim scrubbing tools to detect missing modifiers or mismatched codes.
- Create a checklist for manual review of high-value or complex claims.
- Review claim history for recurring errors and correct root causes.
By building this extra step into your workflow, you can submit cleaner claims that have a higher chance of first-pass approval.
6. Streamline Communication Between Departments
Fragmentation between clinical, administrative, and billing departments often leads to missed or incomplete documentation. Information gaps emerge when providers, coders, and billers aren’t on the same page.
Tips for smoother coordination
- Use secure, shared communication platforms for quick documentation updates.
- Assign liaisons between clinical and billing teams to bridge information gaps.
- Encourage consistent note-taking habits among providers to support accurate coding.
Clear communication is necessary for timely and accurate medical claims management.
7. Monitor Claim Rejections and Denials Closely
Rejections and denials aren’t just setbacks—they’re learning opportunities. Analyzing them can reveal patterns, system flaws, or knowledge gaps in your billing workflow.
Start by
- Categorizing denials (e.g., coding, authorization, eligibility).
- Tracking denial rates monthly and setting internal benchmarks.
- Creating a feedback loop between billing and other departments based on denial insights.
Learning from past claims is a proactive way to improve future submissions.
8. Standardize Documentation Practices
Inconsistent or incomplete documentation often forces billers to make assumptions or submit claims with insufficient justification. That’s risky territory.
Strategies to improve
- Create templates for common procedures to guide provider documentation.
- Use drop-down lists or auto-fill features in your EHR for standard terminology.
- Train providers to link documentation directly to codes and modifiers.
Standardized documentation enhances transparency and supports accurate billing while reducing disputes with payers.
9. Focus on Patient Engagement and Transparency
Sometimes, claims get denied simply because of incorrect or outdated patient-provided information. Therefore, engaging patients early and often can reduce these risks.
What you can do
- Ask patients to review and update their information digitally before each visit.
- Explain their coverage, benefits, and any out-of-pocket costs clearly.
- Let patients track their claims via secure portals.
Empowering patients to participate in their billing process creates a smoother path for accurate medical claims management.
10. Partner with Helixbeat
Not every practice has the bandwidth to manage billing in-house. Outsourcing to experienced medical billing services can take the pressure off internal teams while elevating accuracy levels. Here’s why you should partner with Helixbeat:
1. Specialized Experience in Your Medical Field
Helixbeat covers ICD-10-CM, CPT, and HCPCS standards to minimize claim rejections and maximize reimbursements. With our team of certified coders and robust claim submission workflows, we help healthcare providers reduce delays, stay compliant, and improve cash flow from day one.
2. Proven Success with Similar-Sized Practices
Whether you’re a growing clinic or a large hospital network, Helixbeat has a proven track record of optimizing revenue cycles for healthcare providers of all sizes. Our case studies highlight real-world results, from improved collections to reduced denials.
3. Robust Data Security & HIPAA Compliance
Helixbeat adheres to the highest standards in data protection, including full HIPAA compliance, encrypted data exchange, and regular audits to keep your sensitive information safe.
4. Seamless Integration with EHR & PM Systems
Helixbeat offers seamless integration with leading EHR and Practice Management systems to minimize disruption and facilitate smoother workflows.
5. Dedicated Account Managers & Clear SLAs
With Helixbeat, every client is assigned a dedicated account manager who serves as a single point of contact—backed by service level agreements (SLAs) that clearly define response times, performance benchmarks, and accountability.
6. Transparent Reporting & Real-Time Dashboards
Helixbeat’s intuitive dashboards and transparent reporting provide real-time insights into collections, claims, denials, and key financial KPIs.
Final Thoughts
Improving claims submission accuracy is a strategic move that directly impacts your bottom line, patient trust, and operational efficiency. But you don’t have to tackle it alone.
Partner with Helixbeat—your end-to-end solution for accurate, compliant, and efficient medical claims management. With a team of experts, advanced billing tools, and a commitment to transparency and results, we help healthcare providers submit smarter, get paid faster, and focus more on what matters most: delivering quality care.
Talk to us today and see how we can streamline your claims and transform your revenue cycle.
FAQs
1. Why is accurate medical claims submission important?
Accurate claims submission helps reduce denials, accelerates reimbursement timelines, and improves cash flow. It’s a critical part of medical claims management that helps healthcare providers avoid administrative bottlenecks and maintain financial stability.
2. What are the most common errors in medical claims management?
Frequent issues include incorrect patient details, outdated medical codes, missing documentation, lack of pre-authorization, and eligibility verification errors.
3. What role does coding play in medical claims management?
Coding translates patient diagnoses and procedures into standardized formats (ICD-10, CPT, HCPCS) for billing purposes. Accurate and up-to-date coding helps medical claims get approved faster and supports compliance with payer requirements.
4. What makes Helixbeat a reliable partner for medical claims management?
Helixbeat offers specialized billing services, certified coding experts, real-time dashboards, and seamless EHR integration. These features help healthcare providers streamline operations, reduce claim errors, and improve overall financial performance.