Studies indicate that approximately 30% of healthcare organizations incur financial losses due to issues in their billing and claims processes. The reason for this is that their Revenue Cycle Management (RCM) and Electronic Health Record (EHR) systems don’t work together smoothly.
When these systems are not connected, healthcare providers face delays in payments, claim denials, and extra work, which can affect both patient care and the business side of things.
The solution is to integrate RCM with EHR systems. By connecting patient information with billing details, this integration helps reduce errors, expedite payments, and streamline operations. Here, we’ll show how combining RCM and EHR can fix these issues and improve healthcare operations.
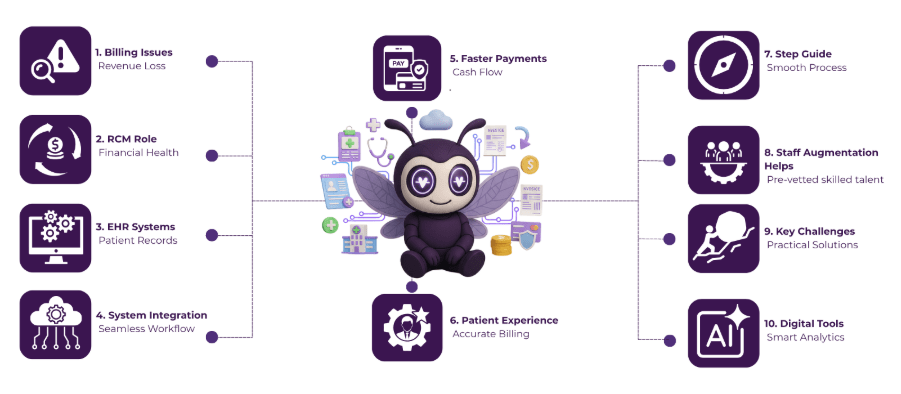
Table of Contents
What is RCM and Why It Matters in Healthcare?
Revenue Cycle Management (RCM) is the process of managing the financial aspects of healthcare services, from patient registration and insurance verification to billing and payment collection.
It makes sure that healthcare providers are paid accurately and on time for their services. RCM is crucial because it helps healthcare organizations maintain financial health, reduce claim denials, and improve cash flow, allowing them to focus on delivering quality care to patients.
The Role of EHR Systems in Storing and Managing Patient Data
RCM services play a vital role in the financial operations of healthcare providers, and they work seamlessly with EHR systems to enhance patient care and administrative efficiency. Here’s how EHR systems contribute to managing and storing patient data:
- Centralized Patient Information: EHR systems store all patient data in one place, including medical history, diagnoses, treatments, and lab results.
- Improved Accessibility: Authorized healthcare providers can access patient records quickly and securely, anytime and anywhere.
- Enhanced Care Coordination: EHRs allow different healthcare providers to share patient information, leading to better-coordinated care.
- Reduced Errors: With accurate and up-to-date data, EHRs help minimize medication errors and duplicate tests.
- Compliance and Security: EHRs are designed to meet regulatory standards, making sure that patient data is secure and protected.
Why Integrating RCM with EHR is Important for Providers and Patients
Revenue cycle management in healthcare plays a critical role in ensuring both operational efficiency and financial stability. By integrating RCM with EHR systems, healthcare providers can address key challenges and enhance overall performance. Here’s why this integration is important for both providers and patients:
1. Streamlined Workflow and Reduced Errors
Integrating RCM with EHR systems reduces manual data entry by up to 70%, leading to fewer errors and discrepancies in patient billing. According to a study, this integration can cut down billing-related errors by 25%, ensuring more accurate and efficient processing of claims.
2. Faster Payments and Improved Cash Flow
By linking RCM with EHR, healthcare organizations can shorten the time it takes to process claims by 30-40%. This means faster payments, with an average reduction of 20% in claim denials, helping providers maintain a steady and predictable cash flow.
3. Better Patient Experience
A survey found that 68% of patients are more satisfied when billing is accurate and transparent. Integrated RCM and EHR systems reduce billing errors and ensure correct processing of insurance details, leading to 15-20% fewer patient complaints regarding billing issues, ultimately improving the overall patient experience.
Step-by-Step Process to Integrate RCM with EHR
An experienced RCM company plays a crucial role in ensuring a smooth integration of Revenue Cycle Management with EHR systems, helping healthcare providers optimize their billing processes. Here’s a step-by-step guide to integrating RCM with EHR:
1. Assess Current Systems and Identify Gaps
Before beginning the integration process, assess the existing RCM and EHR systems to understand their capabilities, limitations, and areas for improvement. This step helps identify gaps in data flow, compatibility issues, or inefficiencies that need to be addressed during integration.
2. Choose the Right Integration Solution
Select an integration platform or software that allows seamless communication between the RCM and EHR systems. This could involve using APIs (Application Programming Interfaces) or middleware to ensure that both systems can exchange data securely and efficiently, minimizing errors in data transfer.
3. Map Data Between RCM and EHR Systems
Data mapping is crucial for integration. Align patient information, billing codes, insurance details, and other relevant data fields between the two systems. This ensures that information flows correctly from EHR to RCM, reducing discrepancies and ensuring accurate billing.
4. Test the Integration
Before going live, perform a series of tests to verify that the integration works as intended. Run test cases that simulate actual patient data transactions, billing processes, and payment workflows to identify any issues. Testing ensures that the systems can handle real-time data exchanges and minimize errors.
5. Train Staff on New Workflow
Once the integration is set up, provide training for healthcare providers and administrative staff. Familiarize them with the new workflows, ensuring they understand how the integrated system works and how to troubleshoot common issues. Proper training helps avoid confusion and ensures smooth adoption of the new process.
6. Monitor and Optimize the Integration
After the integration is live, continually monitor its performance. Track key metrics such as claim approval rates, billing accuracy, and payment cycles. Use this data to make adjustments and improvements, ensuring that both RCM and EHR systems continue to operate at optimal levels for long-term efficiency.
Challenges in RCM & EHR Integration (and How to Overcome Them)
1. Data Compatibility Issues
One of the biggest challenges in RCM and EHR integration is ensuring that both systems can communicate effectively and share data in compatible formats. Different systems may use different data structures, leading to discrepancies or errors during data transfer.
Solution:
To overcome this, ensure that the selected integration solution uses standardized formats, such as HL7 or FHIR, and leverages APIs or middleware that enable seamless data exchange between systems. Regular audits and data mapping exercises can also help prevent compatibility issues.
2. Resistance to Change by Staff
Healthcare providers and administrative staff may resist adopting new systems or workflows, especially if the integration significantly alters their daily tasks. This resistance can slow down the implementation process and affect the success of the integration.
Solution:
Overcome this challenge by offering comprehensive training and support. Involve staff early in the integration process to get their feedback and help them understand the long-term benefits of the integration, such as reduced errors and faster payments.
3. Data Security and Compliance Concerns
Integrating RCM and EHR systems means exchanging sensitive patient data, raising concerns about data privacy, security, and compliance with regulations like HIPAA.
Solution:
To mitigate these concerns, choose integration solutions that comply with industry standards and employ robust encryption methods to secure patient data during transmission. Regularly update security protocols and conduct compliance audits to ensure that the system remains secure and meets regulatory requirements.
How RCM Services and Digital Tools Improve Healthcare Performance
RCM services streamline the entire billing and payment process by automating tasks such as claim submission, coding, and payment tracking. This automation reduces manual errors, speeds up the claims process, and ensures more accurate reimbursements, helping healthcare providers maintain a steady cash flow.
By improving the efficiency of these processes, RCM services allow healthcare organizations to focus more on patient care rather than administrative tasks.
Digital tools, such as AI-powered analytics and real-time reporting, further enhance the performance of RCM services. These tools provide valuable insights into financial data, helping healthcare providers identify trends, optimize billing strategies, and minimize claim denials. By integrating these digital solutions, healthcare organizations can improve both financial health and patient satisfaction, creating a more efficient and effective healthcare environment.
Final Words
Integrating RCM with EHR systems can significantly improve efficiency and financial performance for healthcare providers. It helps speed up billing, reduce errors, and expedite payments, leading to improved cash flow and a more seamless experience for patients.
Helixbeat’s RCM services are here to help healthcare providers manage their revenue cycle more effectively. With our tools and expert support, we ensure that your RCM and EHR systems work seamlessly together, improving both your financial performance and patient care. By choosing Helixbeat, you can focus on caring for patients while we handle the billing and payment processes. Schedule a free consultation call now.
FAQ
1. What is the role of RCM in improving healthcare billing efficiency?
RCM helps streamline the billing process by automating tasks such as insurance verification, claim submission, and payment tracking. It reduces manual work, minimizes errors, and ensures that healthcare providers get paid on time for services rendered.
2. How does integrating RCM with EHR systems reduce claim denials?
When RCM and EHR systems are integrated, the patient information from the EHR system automatically feeds into the RCM system. This reduces human error and ensures that claims are accurate and complete, which leads to fewer claim denials and faster payments.
3. Can RCM services help with revenue forecasting?
Yes, RCM services often include financial reporting tools that help healthcare providers predict future revenue based on historical data. This allows organizations to plan better and make informed decisions about budgeting and resource allocation.
4. What impact does RCM integration have on healthcare compliance?
RCM integration helps healthcare providers stay compliant with regulations like HIPAA by ensuring that patient data is handled securely and that billing processes adhere to industry standards. It also helps reduce the risk of audits and penalties by maintaining accurate, well-documented financial records.
5. How can RCM services benefit small healthcare practices?
For small healthcare practices, RCM services can help streamline the billing process, reduce administrative costs, and improve cash flow. By outsourcing revenue cycle management, smaller practices can focus more on patient care while experts handle the financial operations.














