Chronic diseases have become the worst health crisis in the United States. It harms millions of individuals every day. It places a burden on the US healthcare providers. Conditions such as obesity, hypertension, diabetes, high cholesterol, coronary heart disease, chronic obstructive pulmonary disease (COPD), asthma, chronic kidney disease, cancer, and depression are not only prevalent but also among the most costly and complex to manage.
Number six in ten adults die in the US from chronic diseases. Four in ten adults live with two or more chronic conditions. The Centers for Disease Control and Prevention (CDC) estimate that treating these conditions contributes to 90% of the nation’s annual healthcare expenditure, amounting to approximately $3.8 trillion. The rising prevalence of chronic illnesses highlights an urgent need for comprehensive chronic disease management strategies that address both the medical and systemic challenges these diseases pose.
This is where interoperability in healthcare steps forward as a transformative solution. Enabling seamless data exchange and communication across health systems, interoperability is integral in chronic disease management, enabling healthcare providers, patients, and payers to access the correct information. It results in improved outcomes, better care coordination, and reduced costs.
In this blog, we review the critical role of interoperability in chronic disease management in the US, exploring how it addresses existing challenges and shifts the care landscape for both patients and providers.
Table of Contents
The Need for Better Chronic Disease Management
Managing each patient’s chronic disease remains one of the biggest challenges for US healthcare providers. The main challenges are the complexity and long-term nature of the condition. Consistent care and coordination in hospitals, along with active patient engagement, are needed. However, current surveillance in the healthcare system fails to deliver effective care. Let’s discuss the important challenges among them.
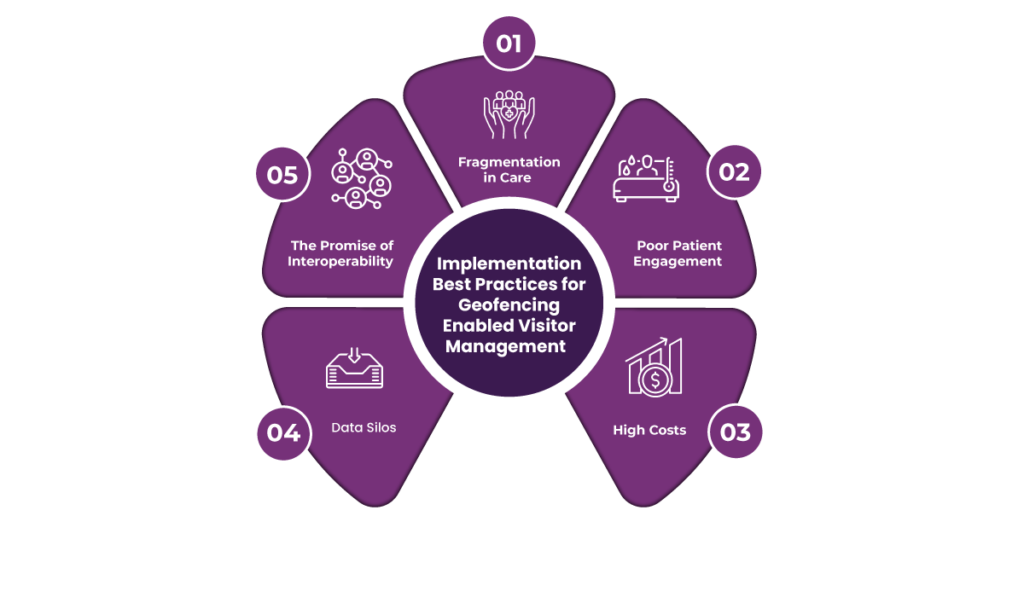
Fragmentation in Care
The most apparent weakness is the fragmentation of the delivery of care. Patients with chronic conditions, for example, may go to several specialists, such as primary care physicians, endocrinologists, cardiologists, and other allied health professionals. However, these providers have no uniform communication pattern, making the care disjointed. For example, a patient’s diabetic records may not be known to a cardiologist, which is why there is an omission in holistic treatment approaches.
This often leads to redundant diagnostic tests, delayed decision-making, and inconsistent treatment plans. The experience can be overwhelming and confusing for patients, which may reduce their trust in the system and their adherence to prescribed treatments.
Poor Patient Engagement
Effective chronic disease management requires active patient collaboration. Many patients remain at the periphery of their care due to a lack of access to their health data. They are often not easily able to view or understand their health records, which further hampers their ability to make informed decisions regarding their conditions.
Furthermore, the unavailability of easy-to-use devices to monitor symptoms, medications, and progress makes patients feel disempowered. Without digital support tools, patients would not be able to monitor the care plans in their minds and would probably miss the earliest warning signs of complications. Poor outcomes lead to further hospitalizations and emergencies due to this lack of engagement.
High Costs
Chronic disease management is costly, indeed. Inefficiency in care delivery, like inappropriate testing and administrative redundancies, increases the costs to both healthcare providers and patients. In the United States, chronic diseases represent 90% of all healthcare expenditures, so chronic diseases are heavy enough for the economy.
Redundant procedures, care delays, and manual data processes inflate costs and divert resources from more impactful interventions. For patients, these inefficiencies translate to higher out-of-pocket expenses, compounding the stress of managing long-term conditions.
Data Silos
One significant barrier to effective chronic disease management is the siloing of healthcare data. Isolated EHRs, laboratory systems, and imaging platforms often make it difficult for critical information to flow smoothly. A common result is that patient histories are unavailable to their providers, which creates lapses in care.
For instance, the history of prescriptions by one provider to a patient is not readily available to another, therefore raising the chance of adverse interactions or contraindications. Integration is not allowed to trace disease course or evaluate treatment efficacy through time.
The Promise of Interoperability
This gives interoperability a stronger power in dealing with all the challenges. It, therefore, helps to make a highly connected ecosystem in which flow is free between providers and systems, between patients, and among them. Its effects include making providers acquire rich patient profiles for delivering relevant care in a consistent fashion. It also empowers the patients with tools for actively engaging with their health for better adherence and outcomes.
The benefits of interoperability are reduced redundancy, cost-effectiveness, and better quality of chronic disease management. These systemic issues would make the healthcare system more patient-centred and efficient in managing chronic conditions.
Understanding Interoperability in Healthcare
What is Interoperability?
Interoperability in healthcare refers to the ability of different information systems, devices, and applications to seamlessly access, exchange, interpret, and use data. It ensures that vital healthcare information flows effortlessly across diverse systems, enabling providers, patients, and other stakeholders to make well-informed decisions.
For example, a cardiologist accessing a patient’s previous tests from a primary care provider’s records can avoid redundant testing and initiate timely interventions.
Interoperability is crucial for improving patient outcomes, enhancing care coordination, and reducing inefficiencies. Without it, healthcare systems remain fragmented, resulting in disjointed care, increased costs, and compromised patient safety. Interoperable systems enable a unified view of patient health data, paving the way for a more efficient and patient-centred approach to care.
Obama’s Concern on Interoperability
During his presidency, Barack Obama highlighted the critical importance of interoperability in transforming the US healthcare system. In 2009, the Health Information Technology for Economic and Clinical Health (HITECH) Act was introduced under his administration to promote the adoption of electronic health records (EHRs). However, Obama later expressed concerns that many EHR systems were not interoperable, effectively creating “digital silos” that hindered information sharing.
In a 2015 speech, Obama emphasized the need for seamless data exchange, pointing out how lack of interoperability led to inefficiencies and compromised care. He criticized EHR vendors for engaging in “information blocking” practices, where systems were designed to limit data sharing, prioritizing competitive advantage over patient welfare.
Obama’s administration pushed for stronger regulations and incentives to achieve interoperability, including the 21st Century Cures Act provisions. These efforts laid the groundwork for improving healthcare data flow and fostering a more connected healthcare ecosystem.
Levels of Interoperability
Interoperability in healthcare operates across multiple levels, each representing a progressive degree of data exchange, understanding, and integration. These levels ensure that healthcare systems, devices, and stakeholders can effectively communicate and utilize shared information.
1. Foundational Interoperability
This is the most basic level, enabling data exchange between systems. It ensures that one system can send data to another, but the receiving system may not interpret or use the data. For example, a lab system may transmit test results to a hospital’s EHR without any standardized formatting.
2. Structural Interoperability
At this level, data is exchanged in a standardized format. The structure and syntax of the data are preserved, ensuring the receiving system can recognize and organize it correctly. For instance, a blood pressure reading is transmitted as a standardized data point with clear systolic and diastolic value parameters.
3. Semantic Interoperability
This level ensures that the exchanged data is recognized and understood. It facilitates meaningful interpretation, allowing systems to use data effectively. For example, a diagnosis of “myocardial infarction” in one system is consistently understood and actionable in another.
4. Organizational Interoperability
Beyond technical aspects, this level addresses governance, workflows, and policies to ensure seamless collaboration among healthcare entities. It aligns system capabilities with organizational objectives for holistic care delivery.
Together, these levels create a robust framework for efficient, patient-centered healthcare.

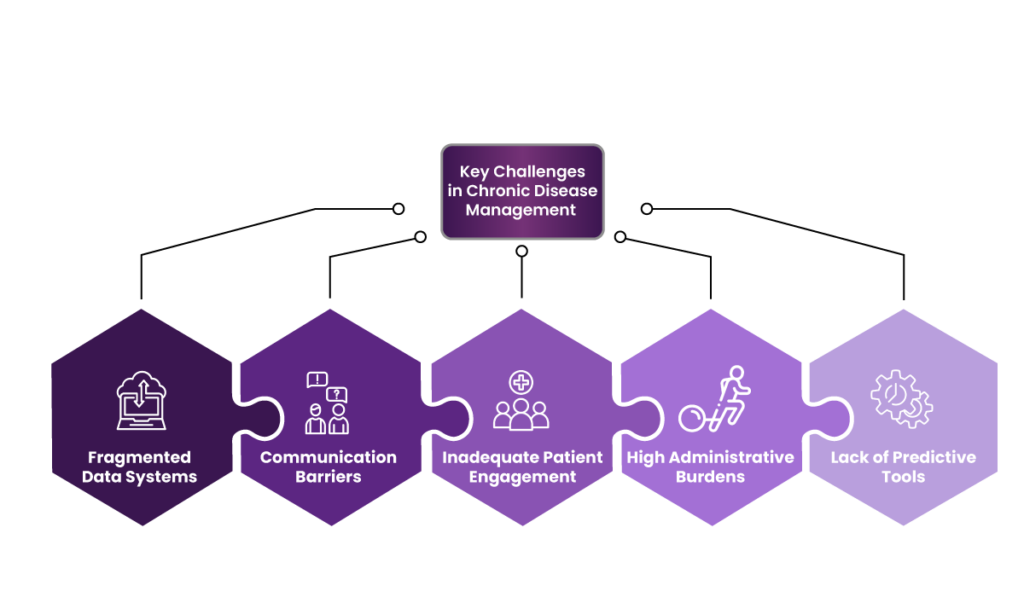
Key Challenges in Chronic Disease Management
Managing chronic diseases presents significant challenges for healthcare providers, patients, and the broader healthcare system. If not addressed, these challenges can lead to poor patient outcomes, inefficiencies, and increased costs, ultimately impacting the sustainability of healthcare businesses.
1. Fragmented Data Systems
Due to fragmented data systems, healthcare providers often face difficulties accessing complete patient information. Patient records are stored across multiple platforms, such as electronic health records (EHRs), diagnostic systems, and pharmacy databases, making creating a unified health profile challenging.
For example, a patient with diabetes and cardiovascular disease may visit different specialists, each maintaining their own records. Without a centralized system, a cardiologist may not have access to the endocrinologist’s recommendations, leading to redundant tests or conflicting treatments.
This fragmentation results in:
- Delayed decision-making.
- Increased medical errors.
- Higher costs for repeated diagnostic tests.
From a business perspective, inefficiencies in data management increase operational costs and reduce patient trust, which can lead to lower retention rates and reputational damage.
2. Communication Barriers
Poor communication among healthcare providers further complicates chronic disease management. Multidisciplinary care, often required for chronic conditions, demands seamless collaboration between primary care physicians, specialists, nurses, and allied health professionals.
For instance, a patient with chronic obstructive pulmonary disease (COPD) may require input from pulmonologists, dietitians, and physical therapists. Without efficient communication channels, coordinating these inputs becomes a logistical challenge.
Communication barriers can lead to:
- Misinterpretation of treatment plans.
- Unnecessary hospital readmissions.
- Reduced patient satisfaction due to inconsistent advice.
These inefficiencies can hurt healthcare organizations financially, as they may face penalties for readmissions under policies like the US Medicare Readmissions Reduction Program.
3. Inadequate Patient Engagement
Chronic disease management heavily relies on patient participation in their care plans. However, many patients remain disengaged due to limited access to their health data, lack of education about their conditions, and inadequate tools to track progress.
For example, a patient with hypertension may miss follow-up appointments or fail to adhere to prescribed lifestyle changes without reminders or real-time feedback on their health metrics.
Inadequate patient engagement results in:
- Poor health outcomes, such as uncontrolled blood pressure or diabetes.
- Increased emergency visits, which strain healthcare resources.
- Higher long-term treatment costs.
Healthcare businesses are also affected, as disengaged patients are less likely to follow through on scheduled visits or procedures, leading to revenue losses.
4. High Administrative Burdens
Administrative tasks, such as manually retrieving patient records, billing, and compliance documentation, significantly increase healthcare providers’ workloads. These burdens take time away from patient care and contribute to provider burnout.
For example, a provider managing a patient with multiple chronic conditions may spend hours coordinating with various insurers and updating fragmented EHR systems.
Consequences of high administrative burdens include:
- Reduced provider productivity.
- Increased operating costs for manual processes.
- Higher staff turnover due to burnout.
For healthcare businesses, these challenges can erode profit margins and decrease overall efficiency, making it harder to scale services or invest in new technologies.
5. Lack of Predictive Tools
Chronic diseases often require proactive management to prevent complications. However, many healthcare providers lack access to predictive analytics tools that can identify early warning signs.
For instance, without predictive insights, a patient with early-stage kidney disease might progress to advanced stages unnoticed, requiring costly dialysis or transplantation.
The absence of predictive tools leads to the following:
- Missed opportunities for early intervention.
- Increased costs for treating advanced conditions.
Healthcare businesses that fail to adopt advanced analytics risk falling behind competitors who offer data-driven care, reducing market competitiveness.
Impact on Healthcare Businesses
The challenges in chronic disease management directly affect healthcare organizations by:
- Increasing costs due to inefficiencies and redundant procedures.
- Damaging patient trust and loyalty due to poor outcomes and service delays.
- Lowering staff morale and retention affects overall care quality.
- Reducing profitability due to penalties, lawsuits, and lower patient retention.
Addressing these challenges through interoperability, predictive tools, and patient-centric strategies can significantly enhance patient outcomes and healthcare organizations’ financial health.
How Interoperability Improves Chronic Disease Management
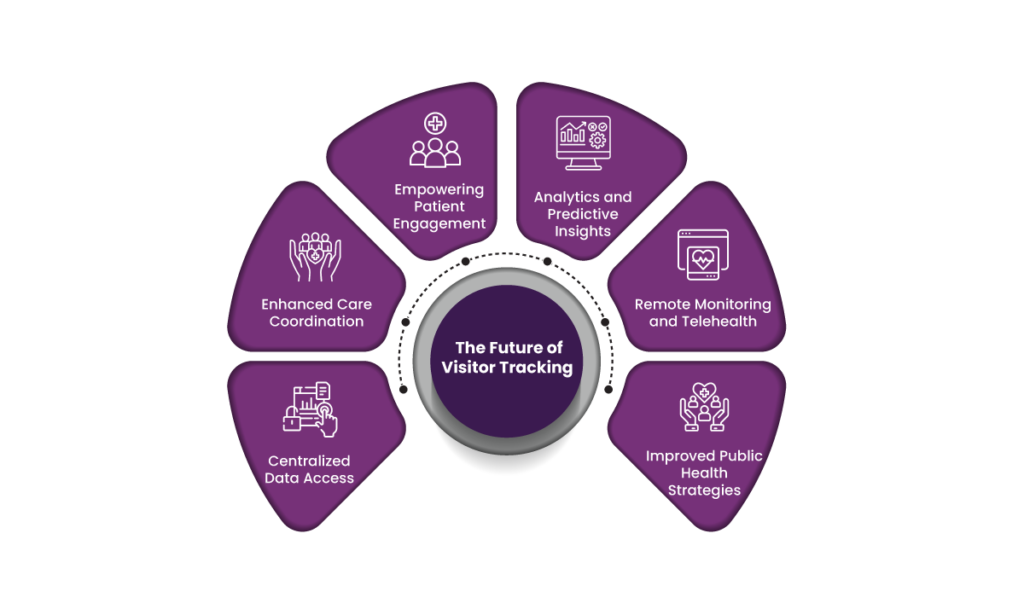
1. Centralized Data Access
Sarah, a 50-year-old diabetic patient, visits Sunrise Medical Center for her routine care. The hospital uses an interoperable electronic health record (EHR) system that integrates data from her primary care physician, endocrinologist, laboratory tests, and pharmacy records into one platform.
Benefits:
- Unified records: Sarah’s complete medical history, including glucose levels, medication adherence, and lab results, is instantly available to her care team.
- Reduced redundancies: Her care team avoids repeating tests, reducing healthcare costs and saving time.
For Sarah, centralized data ensures that her doctor has a holistic view of her condition, leading to personalized and effective care strategies.
2. Enhanced Care Coordination
Chronic disease management often requires collaboration among various specialists. In Sarah’s case, her endocrinologist, cardiologist, and dietitian must align their efforts. Sunrise Medical Center’s interoperable system allows her care team to share real-time updates and communicate seamlessly.
For instance:
- Specialist input: Sarah’s cardiologist notes signs of hypertension during her latest visit, prompting the endocrinologist to adjust her diabetes treatment plan.
- Dietary advice: Her dietitian uploads a revised meal plan to the system, ensuring her endocrinologist is aware of changes that might affect her blood sugar levels.
Interoperability prevents gaps in care, reduces medical errors, and ensures all providers are aligned on treatment objectives.
3. Empowering Patient Engagement
Sarah uses a patient portal connected to Sunrise Medical Center’s interoperable system. This portal allows her to access her health records, set medication reminders, and communicate with her care team.
Examples of engagement:
- Health tracking: Sarah uploads her daily glucose readings to the portal, which her doctor reviews.
- Educational resources: The portal offers tips on diabetes management, such as exercise routines and meal preparation.
By actively involving Sarah in her care, the system fosters adherence to her treatment plan, leading to better outcomes and fewer complications.
4. Analytics and Predictive Insights
Sunrise Medical Center leverages data analytics powered by interoperability to monitor Sarah’s condition and predict potential complications.
For example:
- Trend analysis: If Sarah’s glucose levels consistently trend upward, the system alerts her care team to intervene early.
- Risk predictions: Data patterns indicate Sarah’s likelihood of developing diabetic neuropathy, prompting preventive measures.
Predictive insights empower providers to adopt a proactive approach, minimizing long-term risks and enhancing Sarah’s quality of life.
5. Remote Monitoring and Telehealth
Sarah uses wearable devices, like a continuous glucose monitor, which syncs with Sunrise Medical Center’s EHR system. These devices transmit real-time data, enabling remote monitoring.
For instance:
- If Sarah’s glucose levels spike overnight, an alert is sent to her care team, triggering a telehealth consultation the next morning.
This real-time connectivity ensures Sarah receives timely interventions, reducing hospital visits and improving convenience.
6. Improved Public Health Strategies
Interoperability also aids in population health management. By analyzing aggregated data from diabetic patients like Sarah, Sunrise Medical Center can identify trends and implement community-wide interventions, such as diabetes education workshops.
Fusion: A Transformative Solution for Interoperability in Chronic Disease Management
Chronic diseases, such as diabetes, hypertension, and asthma, affect millions of people worldwide and are a leading cause of long-term healthcare costs and complications. Effective management of these diseases requires continuous monitoring, personalized care, and seamless communication between various healthcare providers, patients, and systems. However, many healthcare systems are fragmented, making it difficult for providers to access all the necessary patient information in real time. Fusion is a transformative solution that enables interoperability across disparate healthcare systems, addressing these challenges by providing a unified platform for managing chronic disease care.
Overview of Fusion’s Features
Fusion is designed to break down the barriers that exist between different healthcare systems, enabling data to flow smoothly across platforms. For chronic disease management, this means that Fusion integrates data from multiple sources, such as electronic health records (EHR), wearable health devices, lab systems, and telemedicine platforms. By supporting industry standards like HL7, FHIR, and IHE, Fusion ensures that patient data can be exchanged accurately and securely, regardless of the system used by healthcare providers or patients.
One of Fusion’s key features is its ability to aggregate data from remote patient monitoring tools, such as glucose meters for diabetes or blood pressure monitors for hypertension. This enables healthcare providers to track patients’ health metrics continuously, making it easier to adjust treatment plans in real-time. Fusion’s real-time data integration reduces the chances of gaps in care, allowing providers to act swiftly and proactively.
Fusion also offers advanced analytics capabilities, providing providers with deep insights into patient data. By analyzing trends and patterns in chronic disease management, healthcare teams can identify patients at risk of complications and intervene early to prevent adverse outcomes. The platform’s customizable dashboards make it easy for healthcare professionals to monitor patient progress, track treatment plan adherence, and evaluate interventions’ effectiveness.
Benefits for Chronic Disease Providers
Fusion offers significant benefits for healthcare providers managing patients with chronic diseases, enhancing the efficiency and quality of care delivered. Below are some key advantages:
- Comprehensive Patient Profiles: Chronic disease management requires a holistic view of a patient’s health. Fusion aggregates data from multiple sources, creating a comprehensive profile that includes medical history, lab results, medication records, and remote monitoring data. This allows providers to understand the full context of a patient’s condition and deliver more personalized care.
- Improved Coordination and Communication: Fusion promotes collaboration across care teams, enabling seamless communication between specialists, primary care physicians, and other healthcare providers. By eliminating data silos, the platform ensures that everyone involved in a patient’s care is on the same page, improving the continuity of care.
- Timely Interventions: With real-time data access, healthcare providers can make timely interventions based on up-to-date health information. Whether adjusting medications, providing lifestyle recommendations, or scheduling follow-up appointments, Fusion allows for rapid responses to changing patient needs.
- Better Patient Engagement: Fusion’s patient-facing features empower individuals to manage their chronic diseases actively. Through personalized health portals and mobile apps, patients can track their own health data, receive medication reminders, and share their progress with their healthcare providers. This active engagement leads to better adherence to treatment plans and improved health outcomes.
- Cost Savings: By improving care coordination, reducing hospital readmissions, and preventing complications, Fusion helps reduce the long-term costs associated with chronic disease management. Healthcare systems can save money by focusing on preventive care and reducing the need for emergency interventions.
- Regulatory Compliance: Fusion complies with health data protection regulations such as HIPAA, ensuring that patient information is secure and confidential. This is especially important for chronic disease management, where sensitive health data is frequently exchanged.
Case Studies
- Case Study 1: Diabetes Management A healthcare network managing a large population of diabetic patients faced challenges in coordinating care across multiple specialists; by implementing Fusion, the network integrated data from EHRs, remote glucose monitors, and pharmacy systems. This allowed endocrinologists, primary care physicians, and dieticians to collaborate more effectively, leading to better glycemic control and reduced complications for patients.
Conclusion
In conclusion, interoperability is essential in the effective management of chronic diseases. Allowing seamless communication between various healthcare systems ensures that patient data is accessible in real time, regardless of the platform used. This integration improves care coordination, reduces the risk of errors, and enables timely interventions.
Fusion facilitates all of your interoperability needs for chronic disease management. Healthcare providers can make data-driven decisions, while patients are empowered to manage their conditions more actively.
Frequently asked question
- What is interoperability in healthcare?
Interoperability refers to the ability of different healthcare systems, devices, and applications to communicate and exchange data seamlessly, ensuring that healthcare providers, patients, and other stakeholders have access to the most up-to-date and complete health information.
- How does interoperability improve chronic disease management?
Interoperability enhances chronic disease management by enabling seamless data sharing among healthcare providers, ensuring better care coordination, reducing redundancies, and providing patients with tools to manage their conditions actively.
- What are the main challenges in managing chronic diseases?
Key challenges include fragmented care, limited patient engagement, high treatment costs, data silos, and inadequate communication among providers, which can lead to delays, errors, and inefficient care.
- How can patients benefit from interoperable healthcare systems?
Patients benefit by having easier access to their health records, being able to engage in their own care, and receiving personalized and coordinated treatment from multiple providers. This can lead to better health outcomes and fewer hospitalizations.
- What role does data play in chronic disease management?
Data is crucial in chronic disease management as it helps track disease progression, monitor treatment effectiveness, predict complications, and support informed decision-making by healthcare providers and patients alike.
- What are the levels of interoperability in healthcare?
The four levels of interoperability are:
- Foundational: Basic data exchange.
- Structural: Data exchanged in standardized formats.
- Semantic: Data is recognized and understood across systems.
- Organizational: Policies, workflows, and governance to support seamless care.
- Why is patient engagement important in chronic disease management?
Active patient engagement leads to better adherence to treatment plans, improved self-management, and early identification of complications, resulting in better health outcomes and fewer emergency visits.
- How does interoperability reduce healthcare costs?
Interoperability streamlines processes by eliminating redundant testing, improving care coordination, and reducing errors, leading to cost savings for healthcare providers and patients.
- What are the economic impacts of chronic disease management on healthcare systems?
Chronic diseases account for a significant portion of healthcare expenditures, with inefficiencies, redundant procedures, and administrative burdens further increasing costs. Effective chronic disease management through interoperability can reduce these economic burdens.
- What are predictive tools, and how do they help in chronic disease management?
Predictive tools use data analytics to identify early warning signs of complications in chronic diseases. They allow healthcare providers to intervene proactively, reducing the likelihood of disease progression and costly treatments down the line.