Integrating patient data management systems (PDMS) with EMRs (Electronic Medical Records) and EHRs (Electronic Health Records) is crucial for improving the efficiency, accuracy, and overall quality of healthcare delivery. While the adoption of digital records has become a standard healthcare practice, the seamless integration of patient data management software into these systems remains a complex challenge for many organizations.
With fragmented data systems, healthcare providers often struggle to achieve a unified view of patient information. This can lead to inefficiencies, errors, and delays in patient care. However, by integrating patient data solutions with EMRs/EHRs, healthcare providers can unlock the potential of streamlined workflows, improved patient engagement, and enhanced clinical decision-making.
Table of Contents
What is the Role of Patient Data Management Systems (PDMS)?
Patient data management systems (PDMS) are digital platforms designed to manage the collection, storage, processing, and exchange of patient data. These systems are essential for tracking patient health records, lab results, medications, and treatment plans.
By integrating PDMS with EMRs and EHRs, healthcare providers can ensure that patient data is easily accessible, secure, and up-to-date across multiple platforms. This integration provides a comprehensive view of the patient’s journey, from appointment scheduling to diagnosis and treatment, enhancing the accuracy of care and minimizing the potential for errors.
See how patient data management systems can streamline your integration with EMRs/EHRs. Get a Free Demo
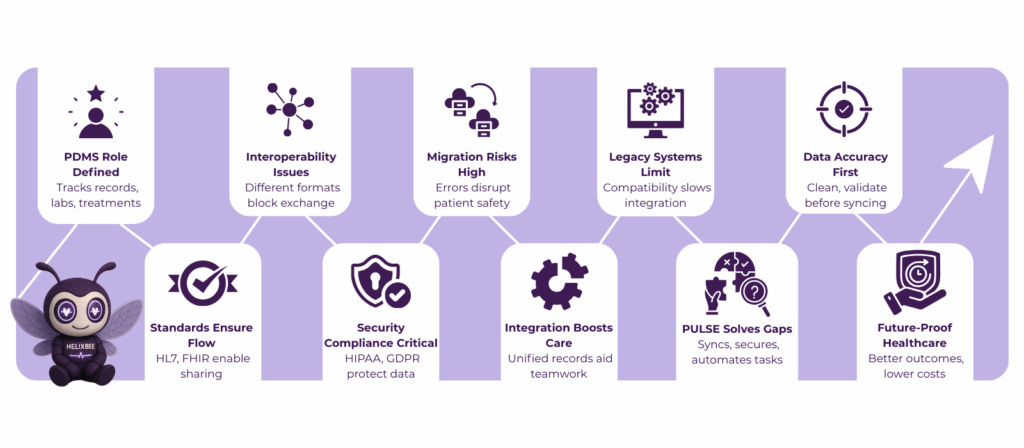
Key Challenges in Integrating PDMS with EMRs/EHRs
Integrating patient data management systems with EMRs/EHRs is not without its challenges. Below are some of the common hurdles healthcare providers face:
- Interoperability Issues
One of the primary challenges of integrating PDMS with EMRs/EHRs is the lack of interoperability between systems. Many EMRs/EHRs use proprietary data formats and communication protocols, making it difficult for different systems to exchange information seamlessly. Achieving true interoperability requires adopting common data standards, such as HL7 or FHIR, to ensure smooth communication between systems.
- Data Migration Challenges
Migrating patient data from one system to another is often a time-consuming and error-prone process. Inaccuracies in the data migration process can lead to incomplete or incorrect patient records, which may compromise patient safety and care. Thorough data validation and mapping are essential to ensure data integrity during migration.
- System Compatibility
Legacy systems may not be compatible with newer patient data management software solutions, leading to integration difficulties. Compatibility issues can hinder the effectiveness of PDMS integration, leading to costly workarounds or system downtimes.
Ready to overcome integration challenges? Start Your Free Trial with PULSE →
Best Practices for Successful Integration of PDMS with EMRs/EHRs
To overcome these challenges, healthcare organizations must adopt best practices when integrating patient data management systems with EMRs/EHRs:
- Ensuring Data Accuracy
Before initiating the integration, healthcare providers should thoroughly clean and validate their existing data. This includes checking for duplicates, errors, and outdated information that could affect patient care. Regular data audits and data quality checks are necessary to maintain accuracy throughout the integration process.
- Adopting Standardized Protocols
Adopting industry-standard data exchange protocols, such as HL7 and FHIR, is crucial for ensuring compatibility between PDMS and EMRs/EHRs. Standardization ensures that data can be shared consistently and accurately across different systems.
- Prioritizing Security and Compliance
Data security is a critical concern when handling sensitive patient information. Compliance with regulations like HIPAA must be prioritized during the integration process. This includes implementing encryption, access controls, and audit trails to protect patient data from unauthorized access and disclosure.
Benefits of Seamless Integration: Improving Healthcare Delivery
Seamless integration of a patient data management system (PDMS) with EMRs/EHRs offers transformative benefits for healthcare providers, patients, and operational workflows. Below are the key advantages explained in detail:
- Improved Care Coordination
Integration ensures that all healthcare teams, physicians, nurses, and administrative staff have access to a unified patient record. This eliminates information silos, allowing clinicians to make informed decisions quickly. With comprehensive, real-time patient data, care coordination improves, leading to faster diagnosis, better treatment planning, and reduced risk of medical errors.
- Enhanced Patient Engagement
When patient records are integrated and easily accessible, patients can receive timely updates, notifications, and follow-up reminders. This strengthens communication between providers and patients, encourages adherence to care plans, and improves overall patient satisfaction. Patients feel more empowered and involved in their healthcare journey.
- Reduced Errors and Data Duplication
Integration eliminates the need for multiple manual entries across different systems. This significantly reduces errors, such as duplicated tests, incorrect prescriptions, or missing medical histories, ensuring that accurate and reliable patient information is consistently available.
- Increased Operational Efficiency
Administrative tasks, such as appointment scheduling, billing, and reporting, are streamlined through integrated systems. This allows staff to focus more on patient care rather than repetitive paperwork, improving the productivity of healthcare facilities and reducing operational costs.
- Data-Driven Decision Making
With seamless integration, healthcare providers can generate real-time reports, track key metrics, and analyze trends effectively. This supports evidence-based decision-making, identifies areas for improvement, and enables better resource allocation across the organization.
- Regulatory Compliance and Security
Integrated systems ensure that sensitive patient data is handled securely and in compliance with regulations such as HIPAA. This minimizes the risk of data breaches, protects patient privacy, and builds trust between providers and patients.
HelixBeat’s PULSE: A Patient Data Management Solution
HelixBeat’s PULSE is designed to address the challenges of modern healthcare data management, offering a fully integrated solution for managing patient records, ensuring interoperability with EMRs/EHRs, and improving operational efficiency. Here are its key features and benefits in detail:
- Real-Time Data Synchronization
PULSE continuously updates patient information across EMRs, EHRs, and PDMS platforms, ensuring that clinicians always have access to the most current patient data. This real-time syncing minimizes errors caused by outdated information and improves decision-making.
- Streamlined Data Migration
Migrating patient data from legacy systems to modern platforms can be complex and error-prone. PULSE provides automated migration tools that validate, map, and transfer data accurately, reducing the risk of data loss or discrepancies during integration.
- Advanced Security and Compliance
Handling sensitive patient data requires stringent security measures. PULSE ensures HIPAA and GDPR compliance through end-to-end encryption, role-based access controls, and detailed audit logs, giving healthcare providers and patients confidence in data safety.
- Interoperability Support
PULSE supports standardized communication protocols such as HL7 and FHIR, enabling seamless integration with a wide range of EMR/EHR systems. This interoperability ensures that healthcare providers can access and share patient information effortlessly, regardless of the system used.
- Automated Workflows and Alerts
Administrative tasks, such as appointment scheduling, lab result notifications, and follow-up reminders, can be automated with PULSE, freeing up staff time and reducing the likelihood of manual errors. Automated alerts ensure critical patient data is acted upon promptly, enhancing care delivery.
- Comprehensive Analytics and Reporting
PULSE provides detailed analytics on patient data, workflow efficiency, and care outcomes. Healthcare providers can utilize these insights to make informed decisions, identify bottlenecks, and continually optimize processes to enhance patient care.
- Mobile and Remote Access
The platform is accessible via mobile devices, enabling healthcare providers to access patient data anytime, anywhere. This flexibility is beneficial for multi-location practices and telehealth services, ensuring continuity of care.
Key Takeaways
Integrating patient data management systems with EMRs/EHRs presents significant challenges. Still, by adopting best practices and leveraging the right tools, healthcare providers can overcome these obstacles and unlock the full potential of digital healthcare solutions. PULSE by HelixBeat provides the tools necessary to streamline integration, ensuring better care coordination, improved patient engagement, and enhanced operational efficiency.
By investing in patient data management software that prioritizes interoperability, data accuracy, and security, healthcare providers can improve patient outcomes and drive the future of healthcare.
Transform your patient data management system today with PULSE. Sign Up for a Demo
FAQs
- What is a patient data management system?
A patient data management system (PDMS) enables healthcare organizations to manage, store, and process patient data securely, ensuring that patient information is accurate and readily accessible.
- Why is interoperability important in EHR systems?
Interoperability ensures that patient data can be shared seamlessly between different systems, improving care coordination and reducing the risk of errors due to fragmented information.
- What challenges are associated with EHR integration?
Common challenges include data migration errors, system compatibility issues, and the complexity of achieving full interoperability between different platforms.
- How can PULSE assist with EHR integration?
PULSE offers seamless integration with EMRs/EHRs, ensuring real-time syncing of patient data and compliance with healthcare regulations.
- What is the biggest challenge in implementing EHR systems?
The biggest challenge is achieving interoperability between legacy systems and modern healthcare platforms, which often use different data formats and protocols.
- How can PULSE help with data migration?
PULSE offers tools to ensure smooth and accurate migration of patient data from legacy systems to new platforms, minimizing the risk of errors.
- What are the security features of PULSE?
PULSE includes end-to-end encryption, role-based access controls, and audit trails to ensure that patient data is secure and HIPAA-compliant.
- How does PULSE improve operational efficiency?
By automating administrative tasks and enabling seamless data sharing, PULSE reduces manual work, allowing healthcare providers to focus more on patient care.
- Can PULSE integrate with existing healthcare systems?
Yes, PULSE supports integration with a variety of EMR/EHR systems using standardized protocols like HL7 and FHIR.
- How long does it take to integrate PULSE with EMRs/EHRs?
Integration times vary depending on the complexity of the existing systems, but PULSE is designed for quick and efficient deployment.
- Does PULSE support mobile access?
Yes, PULSE offers a mobile-optimized interface, allowing healthcare providers to access patient data and manage workflows on the go.
- What are the key benefits of using PULSE for EHR integration?
PULSE offers seamless integration, improved data accuracy, enhanced patient engagement, and streamlined workflows, leading to better patient care and operational efficiency.