Behind every successful healthcare organization lies a system that keeps financial operations running smoothly—medical coding and revenue cycle management (RCM). These two elements dictate how efficiently providers get paid, how accurately patient data is recorded, and how seamlessly claims are processed.
Medical coding converts diagnoses, treatments, and procedures into universal codes that facilitate billing, insurance claims, and financial reporting. Systems like ICD-10-CM, CPT, and HCPCS are the foundation of this process, linking clinical care with reimbursement. When integrated with revenue cycle management services, these codes reduce claim denials and help healthcare providers optimize cash flow and financial performance.
Table of Contents
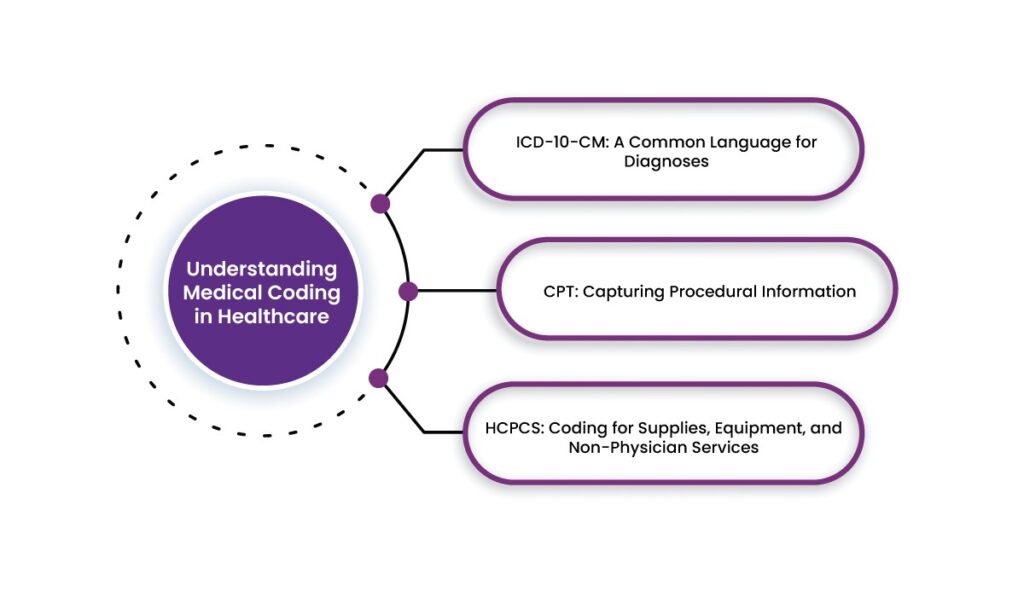
Understanding Medical Coding in Healthcare
1. ICD-10-CM: A Common Language for Diagnoses
The ICD-10-CM coding system plays a key role in standardizing diagnoses. By assigning a unique alphanumeric code to each condition, this system creates a universal language that supports accurate medical records, streamlined claims processing, and improved patient care.
For example, a patient diagnosed with Type 2 diabetes with kidney complications—under ICD-10-CM, this condition is coded as E11.22.
From public health tracking to revenue cycle management, ICD-10-CM facilitates efficient data collection that benefits hospitals, insurers, and research institutions alike.
2. CPT: Capturing Procedural Information
Every medical procedure, from a simple flu shot to a major surgery, needs a standardized way to be recorded. That’s where the Current Procedural Terminology (CPT) codes come in. Developed by the American Medical Association (AMA), these five-digit codes create a universal language for healthcare professionals, insurance companies, and billing departments.
For example, if a patient visits their doctor for a routine checkup, the visit might be coded as 99213 under CPT. This standardization helps eliminate confusion and makes it easier for healthcare providers to communicate procedural details clearly.
By using the correct codes, healthcare organizations can avoid billing errors, minimize claim denials, and streamline revenue cycle management.
3. HCPCS: Coding for Supplies, Equipment, and Non-Physician Services
The Healthcare Common Procedure Coding System (HCPCS) complements CPT coding, incorporating alphanumeric codes for supplies, durable medical equipment (DME), and services not covered under CPT. For example, if a patient requires a powered wheelchair for mobility support, it is billed under HCPCS code E1130.
HCPCS enables proper billing for non-physician services and facilitates claims processing for government payers like Medicare and Medicaid.
The Connection Between Coding and Revenue Cycle Management
Accurate medical coding is integral to revenue cycle management (RCM), which includes all administrative and financial processes from patient registration to final payment collection. Proper coding translates healthcare services into billable claims and reduces claim rejections or financial losses.
Key Stages of Revenue Cycle Management
1. Patient Registration & Insurance Verification
a. Before any procedure, healthcare facilities collect patient demographic and insurance details.
b. Accurate data entry prevents issues related to denied claims.
2. Medical Documentation & Coding
a. Physicians document diagnoses and procedures, which medical coders assign with ICD-10-CM, CPT, and HCPCS codes.
b. Any discrepancies in documentation can result in coding errors and affect reimbursement.
3. Charge Capture & Claims Submission
a. The assigned codes are translated into claims and submitted to insurance payers for reimbursement.
4. Claims Adjudication & Payment Processing
a. Insurance companies review claims, approve or deny payment, and communicate discrepancies.
5. Denial Management & Revenue Optimization
a. A dedicated team reviews denied claims, identifies patterns, and rectifies issues in coding and billing.
b. Preventive measures, such as audit mechanisms, enhance efficiency.
6. Patient Billing & Collections
a. Once insurance payments are settled, patients receive statements for any outstanding balances.
b. Clear and accurate billing promotes patient trust and minimizes disputes.
Medical Coding & Billing by Helixbeat
As part of the comprehensive RCM service, our expert coding solutions simplify claim processing, reduce rejections, and help healthcare providers achieve faster, more accurate reimbursements without the hassle.
Precision-Driven Coding for Maximum Reimbursement
At Helixbeat, our certified coding specialists meticulously apply ICD-10-CM, CPT, and HCPCS codes to capture every procedure, diagnosis, and service with complete accuracy. Similarly, with constantly evolving regulations, we keep up with payer requirements, so providers don’t have to worry about rejected claims due to outdated codes or missing details.
Faster Claims Processing, Fewer Denials
Our services support a seamless flow from patient encounters to reimbursement, thus helping healthcare organizations maintain steady cash flow and optimize revenue recovery.
Why Helixbeat Stands Out?
a. Certified experts in ICD-10-CM, CPT, and HCPCS coding
b. Accurate documentation that meets compliance and regulatory standards
c. Seamless claims processing to reduce denials and speed up reimbursements
d. Integrated into our full-spectrum RCM services for financial efficiency
With Helixbeat handling your medical coding and billing, healthcare providers can focus on patient care while experiencing a smoother, more profitable revenue cycle.
Final Thoughts
Medical coding isn’t just about assigning the right codes—it’s the foundation of efficient revenue cycle management (RCM). With ICD-10-CM streamlining disease classification, CPT standardizing procedural reporting, and HCPCS supporting claims for medical supplies and services, a well-structured coding framework keeps financial operations running smoothly.
As the healthcare industry grows more complex, coding accuracy and a well-optimized RCM process will be the key to financial success and quality patient care. However, to keep up with evolving regulations and payer requirements, healthcare organizations need more than just basic coding knowledge.
With Helixbeat, providers can access expert medical coding, seamless claims processing, and a stronger financial foundation. Let Helixbeat handle the complexities of revenue cycle management—so you can focus on what matters most: patient care.
Get started with Helixbeat today and take control of your revenue cycle!
FAQs
1. What is the role of medical coding in healthcare?
Medical coding translates diagnoses, procedures, and treatments into standardized codes (ICD-10-CM, CPT, HCPCS) used for billing, insurance claims, and financial reporting.
2. How does revenue cycle management (RCM) benefit healthcare providers?
RCM streamlines the financial process from patient registration to final payment collection, helping providers reduce claim denials, optimize reimbursements, and maintain steady cash flow.
3. What are ICD-10-CM, CPT, and HCPCS codes used for?
- ICD-10-CM: Classifies diseases and medical conditions.
- CPT: Standardizes medical procedures and services.
- HCPCS: Covers medical supplies, durable equipment, and non-physician services.
4. Why is accurate coding essential for claim approvals?
Incorrect or incomplete coding can lead to claim rejections, payment delays, and financial losses. Precise coding minimizes errors and improves reimbursement rates.
5. What happens if a claim is denied due to coding errors?
Denied claims undergo a review process where errors are identified and corrected before resubmission. Preventative measures, such as audits, help reduce future denials.
6. How does the medical coding service from Helixbeat improve financial performance?
Helixbeat applies expert coding practices to reduce billing errors, speed up claims processing, and maximize revenue recovery as part of its comprehensive end-to-end RCM service.
7. How does patient registration impact revenue cycle management?
Accurate collection of patient information, including insurance verification, prevents claim denials and billing discrepancies later in the process.
8. What are the key steps in the revenue cycle?
The revenue cycle includes patient registration, coding and charge capture, claims submission, adjudication, denial management, and final payment collection.
9. Why should healthcare providers partner with Helixbeat for RCM services?
The end-to-end RCM services from Helixbeat integrate expert medical coding, seamless claims processing, and financial optimization—allowing providers to focus on patient care while improving revenue stability.