A modern patient record management system plays a direct role in the speed, accuracy, and safety of clinical decisions. Yet, many healthcare providers still rely on outdated methods, putting both patients and operations at risk.
In this blog, we’ll explain why now is the time to upgrade your system, the hidden costs of sticking with legacy tools, and how PULSE by Helixbeat provides a more innovative, scalable, and compliant approach to managing patient records effectively.
From missed diagnoses due to incomplete data to rising medico-legal risks, outdated systems put both providers and patients at risk. According to the American Health Information Management Association (AHIMA), hospitals lose millions annually due to inefficiencies in managing records.
This blog explores why it’s time to upgrade, what features to look for, and how platforms like PULSE by Helixbeat are reshaping health record management for a brighter, safer future.
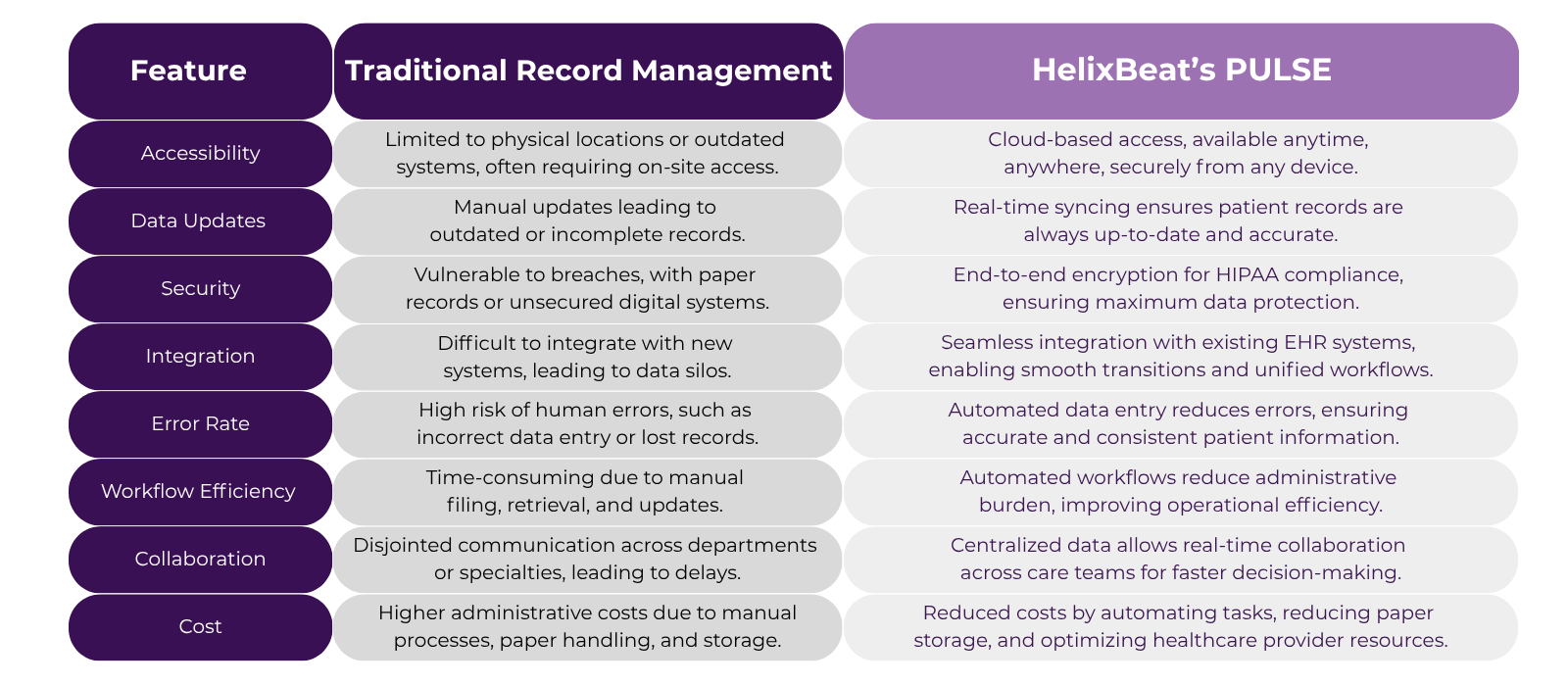
Table of Contents
What Is a Patient Record Management System?
Think of a patient record management system as the central nervous system of your healthcare organization. It’s not just a digital filing cabinet—it’s a living, breathing tool that helps patient care at every point of contact. From front-desk check-in to follow-up appointments, this system captures and combines essential information, enabling better care delivery.
Instead of concentrating exclusively on documentation, a modern system:
- Synchronizes data across departments (labs, pharmacy, radiology, billing)
- Offers real-time visibility into patient status
- Reduces administrative repetition and manual entry
- Flag inconsistencies and alert care teams proactively
Whether cloud-based or on-premise, these systems integrate with electronic medical records or management software to create a seamless and dynamic clinical experience.
The primary purpose of a patient record is to serve as a dynamic, continuous narrative of a person’s health journey. It’s not just a log of medical events—it’s a decision-making tool that drives safe, personalized, and efficient care.
Main Purpose of a Patient Record
A well-maintained patient record enables:
- Clinical continuity – Providers can track changes in symptoms, treatments, and diagnostics across time and specialists.
- Informed decision-making – Clinicians can make faster and more accurate choices when they have access to structured data.
- Patient empowerment – Digital records enable patients to view their medical history, test results, and prescriptions, thereby enhancing transparency and trust.
- Legal and administrative value – Records serve as formal documentation in medico-legal cases, insurance audits, and billing reconciliation.
Common Issues with Outdated Health Record Management
Outdated health record systems, whether paper-based or legacy digital platforms, pose significant risks to clinical efficiency, regulatory compliance, and patient safety. Below is a breakdown of the most pressing issues healthcare providers face when using such systems:
1. Data Retrieval Delays
- Searching through paper files or poorly indexed digital systems can slow down access to critical information.
- This causes bottlenecks during consultations, emergencies, and follow-ups.
2. Incomplete or Missing Patient Information
- Older systems often suffer from poor data consolidation.
- Essential test results or prescriptions may be scattered across systems or missing entirely.
3. Poor Interdepartmental Communication
- Lack of integration between departments (e.g., lab, radiology, and billing) leads to duplication and miscommunication.
- Care becomes fragmented, especially in multi-disciplinary or multi-location setups.
4. Higher Risk of Human Error
- Manual documentation increases the chance of misreading handwriting or skipping essential information.
- Errors in prescriptions, allergies, or diagnostic records can jeopardize patient safety.
5. Lack of Real-Time Updates
- Updates often occur at the end of the day or are delayed until after visits, which can affect accuracy and timeliness.
- Clinicians may make decisions based on outdated information.
6. Administrative Overload
- Manual data entry is time-consuming and error-prone.
- Staff waste valuable hours on repetitive documentation instead of focusing on patient interactions.
7. Compliance and Audit Vulnerabilities
- Legacy systems often lack automated audit trails or encryption.
- This increases the risk of non-compliance with HIPAA and other data protection standards.
8. No Remote Accessibility
- Physicians and admin teams can’t access records remotely, limiting telehealth and off-site decision-making.
- This is especially problematic in emergency and after-hours situations.
9. No Support for Clinical Data Analytics
- Outdated systems don’t capture data in structured formats that can power predictive insights.
- Healthcare organizations lose the opportunity to track outcomes or plan preventive interventions.
10. Difficulties in Scaling
- Legacy systems can’t handle high patient volumes, multi-specialty requirements, or multi-location synchronization.
- As the organization grows, the system becomes a bottleneck.
11. Higher Costs in the Long Run
- Despite seeming cost-effective upfront, outdated systems incur costs through inefficiency, delays, and frequent maintenance.
- Errors, compliance failures, and administrative burdens silently drain financial resources.
12. Patient Dissatisfaction
- Patients expect quick, digital interactions, such as appointment reminders or e-prescriptions.
- Delays and a lack of transparency reduce trust in the quality of care.
Signs It’s Time to Upgrade Your Patient Record Management System
If any of the following issues sound familiar, it’s time to consider a digital transformation:
- Frequent data loss or retrieval delays
- High rates of documentation errors
- Inefficient workflows with paper charts or disconnected software
- Limited remote access for doctors and staff
- Lack of compliance readiness for audits or reporting
- Poor integration with EHRs, billing systems, or pharmacy platforms
Role of Electronic Medical Record in Modern Practices
Here’s a closer look at how EMR and record management software transform everyday clinical practice:
Centralized and Accessible Patient Information
- All patient data—demographics, clinical notes, test results, medications—are stored in one secure location.
- Providers can quickly access a patient’s complete medical history during consultations or in emergencies.
Streamlined Clinical Workflows
- Automated appointment reminders and check-in processes reduce no-shows.
- Integrated templates and note-taking tools speed up consultations and documentation.
Improved Interoperability
- Seamless sharing of information across departments, specialties, and even external providers.
- Enhances care coordination among GPs, specialists, laboratories, and pharmacies.
Real-Time Data Entry and Monitoring
- Clinicians can update patient data on the go using tablets, voice-to-text tools, or desktop dashboards.
- Reduces lag in treatment updates and improves accuracy.
Built-In Decision Support Tools
- Alerts for drug interactions, allergies, and abnormal test values.
- Clinical guidelines and pathways are integrated within the interface.
Automated Reporting and Analytics
- Instant generation of reports for audits, insurance, and compliance.
- Supports population health tracking and quality improvement.
Improved Billing and Revenue Cycle Management
- Automatic coding suggestions reduce billing errors.
- Quicker insurance claims processing leads to faster reimbursements.
Enhanced Compliance and Security
- HIPAA-compliant data handling with encryption, audit trails, and role-based access.
- Reduces legal risk and builds trust with patients.
Supports Remote and Telehealth Capabilities
- Doctors can access EMRs securely from home or mobile devices.
- Facilitates virtual consultations with full access to patient records.
Scalable and Customizable for Practice Growth
- Modular features can be added as the practice grows (e.g., telemedicine, e-prescriptions, lab integration).
- Custom templates for different specialties ensure flexibility.
Tips for a Smooth Transition to a New System
Upgrading doesn’t have to mean disruption. Follow these tips:
- Assess current gaps and define upgrade goals
- Engage stakeholders early—from doctors to IT teams
- Train teams incrementally using mock scenarios
- Start with a pilot group, then scale up
- Track key KPIs like error rates, appointment efficiency, and documentation speed
To Sum It Up
What is the importance of maintaining accurate records in the healthcare system? Records serve as the roadmap for every patient’s journey—from initial consultation to healing and follow-up. Without accuracy, accessibility, and structure, even the best medical teams are left in the dark.
Upgrading your patient record management system improves compliance, streamlines operations, and most importantly, drives better outcomes.
CTA: Ready to future-proof your training? [Explore how PULSE by Helixbeat can transform your record-keeping.]
FAQs
What is the importance of keeping records in the healthcare system?
It ensures continuity of care, legal protection, better diagnosis, and accurate billing.
What is the importance of management in an electronic health record system?
Proper management improves efficiency, enhances data security, and helps comply with healthcare regulations.
How can hospitals modify their record keeping systems to enhance patient care?
By adopting digital platforms, training staff, integrating systems, and enabling patient access to information.
What is the main purpose of a patient record?
To document and guide the patient’s health journey and support clinical decision-making.
What are the key features of a modern patient record management system?
Cloud access, interoperability, security controls, real-time updates, and analytics tools.
How does electronic software improve clinical data accuracy?
By reducing manual errors, providing real-time checks, and enabling structured data input.
Can upgrading your system reduce patient wait times?
Yes, by streamlining administrative workflows and allowing quicker access to patient information.
What are the risks of not upgrading your medical records management tools?
Data breaches, compliance failures, inefficiencies, and lower patient satisfaction.
Is it hard to migrate from paper-based to digital records?
Not with the right platform—PULSE offers phased migration, training, and support.
What security features should I expect in a digital platform like PULSE?
Role-based access, encryption, secure cloud hosting, and real-time monitoring tools.