Today, healthcare systems are generating more data than ever—thanks to electronic health records (EHRs), lab platforms, imaging software, fitness wearables, telemedicine tools, and beyond. But here’s the catch: much of this information remains locked away in isolated systems, creating what’s commonly known as “healthcare data silos.”
These disconnected pockets of data make it difficult to see the full picture of a patient’s health journey. The result? Repeated tests, communication breakdowns, delayed diagnoses, and, in some cases, a decline in care quality. That’s where multi-protocol integration steps in. By connecting scattered systems and breaking down these silos, it paves the way for truly integrated healthcare.
Table of Contents
What Is Multi-Protocol Integration?
Multi-protocol integration refers to the use of various communication protocols and standards to connect disparate healthcare systems, enabling seamless data exchange regardless of their underlying infrastructure. It allows hospitals, clinics, diagnostic labs, and even patient-owned devices to communicate in a language that all systems understand.
The key protocols involved in healthcare data exchange include:
- HL7 (Health Level Seven): One of the oldest and most widely adopted standards for clinical data exchange.
- FHIR (Fast Healthcare Interoperability Resources): A newer, more flexible protocol developed by HL7 to simplify data sharing using web-based APIs.
- DICOM (Digital Imaging and Communications in Medicine): Standard for storing and transmitting medical imaging information.
- X12: Commonly used for administrative and billing data.
- RESTful APIs & JSON/XML: Widely used in modern software for integrating with cloud-based platforms and mobile applications.
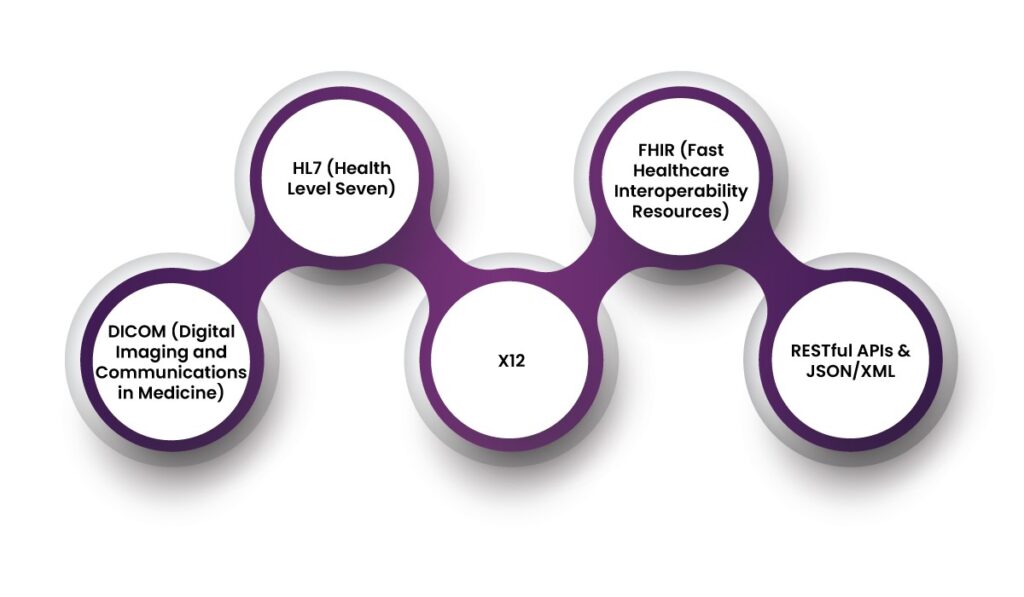
By combining these standards in a single integration layer, healthcare providers can break down silos and support integrated healthcare.
The Role of Multi-Protocol Integration in Integrated Healthcare
Integrated healthcare focuses on delivering patient-centric care by bringing together services across the healthcare continuum—ranging from primary care and specialists to diagnostics and rehabilitation. For this model to succeed, all players in the ecosystem must have access to consistent, accurate, and up-to-date patient information.
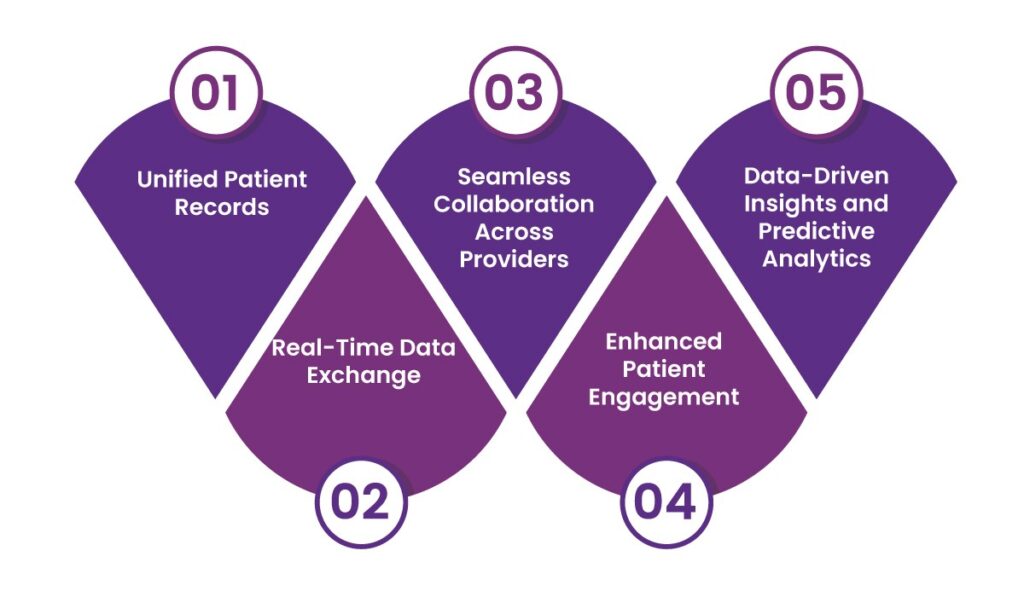
Here’s how multi-protocol integration plays a vital role in achieving that goal:
1. Unified Patient Records
Multi-protocol integration allows data from different systems to be combined into a single, unified patient record. Whether a provider uses HL7 for clinical records, DICOM for radiology, or FHIR for mobile apps, integration platforms normalize this data for real-time access.
This consolidated view helps doctors and specialists see the full picture of a patient’s health—past surgeries, medication history, allergies, lab results, and more—leading to better diagnoses and treatment plans.
2. Real-Time Data Exchange
When patients are treated in emergency situations or transferred between departments, timely access to health information can make all the difference. Multi-protocol integration supports real-time data sharing, enabling clinicians to instantly retrieve information across different systems.
This speed not only supports more responsive care but also reduces administrative bottlenecks that delay treatment.
3. Seamless Collaboration Across Providers
One of the pillars of integrated healthcare is collaboration. Patients today often interact with a diverse set of providers—primary care physicians, dieticians, therapists, etc. Without integrated systems, each provider may operate in a vacuum.
Multi-protocol integration fosters communication between these different players, enabling cross-provider data sharing and coordinated care pathways. This leads to smoother transitions for patients and reduces errors from miscommunication.
4. Enhanced Patient Engagement
Modern patients expect transparency, convenience, and access. Mobile health apps, wearable devices, and patient portals allow individuals to track their vitals, appointments, and prescriptions. These tools often use FHIR or RESTful APIs to connect with larger healthcare networks.
Healthcare systems can connect these consumer-facing platforms with backend clinical systems by incorporating multi-protocol integration. This empowers patients to be active participants in their care journeys.
5. Data-Driven Insights and Predictive Analytics
Integrated data facilitates more than just care delivery—it opens doors for advanced analytics and population health management. When data from various protocols is harmonized, healthcare providers can apply machine learning models to predict disease risk, recommend preventive measures, and identify treatment gaps.
From early detection of chronic illnesses to minimizing readmission rates, data-driven strategies thrive on the kind of interoperability multi-protocol integration offers.
Tackling Technical and Operational Barriers with AERIS
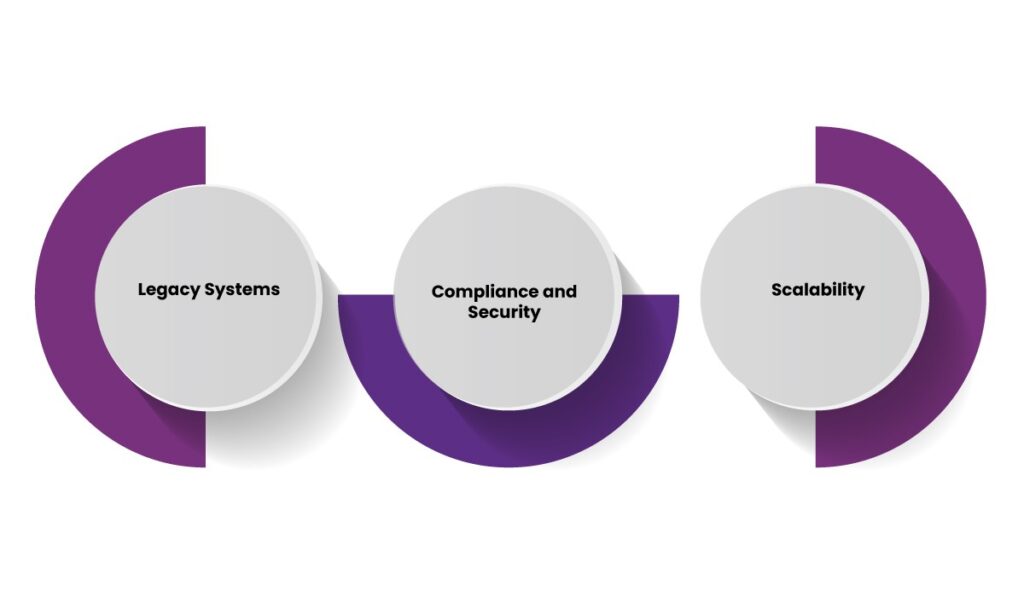
Implementing multi-protocol integration in healthcare is no small feat. Organizations often face several hurdles on the path to integrated healthcare:
- Legacy Systems: Many hospitals and clinics still rely on outdated software that doesn’t natively support modern standards like FHIR. This creates compatibility issues and slows down data sharing.
- Compliance and Security: With sensitive patient data in play, any exchange must align with stringent regulations like HIPAA or the 21st Century Cures Act. Therefore, strong data protection measures are non-negotiable.
- Scalability: As digital health ecosystems expand, integration systems must handle higher data volumes and more endpoints—without delays or breakdowns.
This is where AERIS, a FHIR-based adaptive exchange interoperability system, plays a vital role. AERIS bridges gaps between legacy and modern systems by translating multiple data formats into FHIR, eliminating the need for extensive redevelopment. It offers built-in security features, which help organizations maintain data privacy and meet compliance mandates with confidence. Plus, its adaptive architecture supports seamless scaling, enabling health networks to expand their connectivity without compromising efficiency.
By simplifying complex data exchanges, AERIS lays a strong foundation for integrated healthcare—connecting hospitals, labs, clinics, and digital health platforms into a unified, interoperable ecosystem.
The Future of Integrated Healthcare
As healthcare systems continue to embrace digital transformation, the demand for interoperability will only grow. Technologies like Artificial Intelligence, Internet of Medical Things (IoMT), and Remote Patient Monitoring will further diversify the data landscape.
Multi-protocol integration will be the backbone that ties it all together, allowing disparate systems to communicate without friction. More importantly, it will help shift the healthcare paradigm from reactive to proactive, from isolated interventions to longitudinal care journeys.
Cloud-native integration platforms, smart health exchanges, and no-code interface builders are already making this transformation more accessible. As more healthcare institutions invest in these tools, the dream of integrated healthcare—personalized, connected, and continuous—comes closer to reality.
Final Thoughts
Healthcare data silos have long stood in the way of efficient and patient-centered care. By embracing multi-protocol integration, the industry can unlock the full potential of its digital ecosystem. If you’re looking to unify your healthcare data across systems and standards, AERIS helps healthcare providers, payers, and third-party vendors streamline interoperability—fast, securely, and at scale.
Contact us today and discover how AERIS can transform your data exchange.
FAQs
1. What is integrated healthcare, and why is it important?
Integrated healthcare is a coordinated approach to patient care that connects services across different providers, departments, and systems. It’s important because it promotes better communication, improves patient outcomes, and reduces redundant procedures.
2. What is multi-protocol integration in healthcare?
Multi-protocol integration involves connecting various healthcare systems using a combination of communication standards like HL7, FHIR, DICOM, and X12. This allows different platforms to exchange data seamlessly, contributing to integrated healthcare.
3. Which healthcare standards are commonly used for integration?
Common standards include HL7 for clinical data, FHIR for API-based access, DICOM for medical imaging, X12 for billing, and RESTful APIs for modern applications. Combining these helps create a more integrated healthcare infrastructure.
4. What role does AERIS play in achieving integrated healthcare?
AERIS is a FHIR-based interoperability solution that connects legacy and modern systems by translating various data formats. It helps organizations scale their integration efforts while maintaining security and regulatory alignment.