Today, the ability to seamlessly share and utilize patient data across different platforms, providers, and organizations has become a critical factor in improving patient care.
In this blog, we’ll explore why interoperable healthcare systems matter, the challenges faced when implementing them, and how a tailored approach unlocks their full potential.
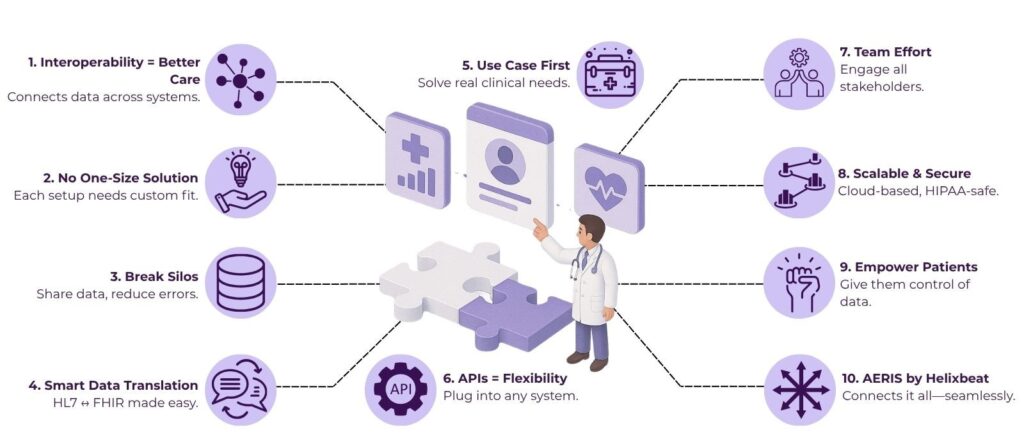
Table of Contents
Why Interoperability is the Backbone of Modern Healthcare
Healthcare today generates massive volumes of data—from electronic health records (EHRs) and lab results to imaging, prescriptions, and metrics from wearable devices. These data points hold invaluable insights to support diagnosis, treatment, and patient management. However, the value of this data often remains trapped in isolated systems that don’t communicate effectively.
Interoperable healthcare systems break down these silos, allowing different healthcare IT systems to exchange, interpret, and use data in meaningful ways. Here’s how the benefits ripple through the entire care continuum:
- Improved patient outcomes: Care teams have access to comprehensive, up-to-date information, which reduces errors and duplications.
- Streamlined workflows: Automated data exchange cuts manual entry, saving time for clinicians.
- Better population health management: Aggregated data enables public health monitoring and research.
- Cost reduction: Avoiding redundant tests and procedures lowers healthcare spending.
According to a 2023 report by MarketsandMarkets, the healthcare interoperability market is projected to reach $1.9 billion by 2028, reflecting the growing demand for connected health systems.
The Pitfalls of One-Size-Fits-All Interoperability
Despite the clear benefits, many healthcare organizations face frustration when attempting to implement interoperable systems. One key reason lies in adopting a one-size-fits-all approach—assuming a single solution or standard can work seamlessly across all settings.
1. Diverse Stakeholders and Systems
Healthcare involves numerous stakeholders: hospitals, clinics, labs, pharmacies, payers, public health authorities, and patients themselves. Each operates unique systems, workflows, and data standards. For example, a large urban hospital may use a comprehensive EHR system like Epic or Cerner, while a small rural clinic relies on a simpler, cost-effective platform.
2. Regulatory and Privacy Considerations
Different regions enforce diverse data protection regulations like HIPAA in the US or GDPR in Europe. Therefore, interoperable systems must be flexible enough to comply with these laws without hindering data sharing.
3. Technical and Infrastructure Gaps
Some healthcare providers may lack the technological infrastructure to adopt complex interoperability solutions, which can result in uneven progress.
How to Adopt a Flexible Interoperability Strategy
To build truly effective interoperable healthcare systems, organizations must adopt a flexible strategy that acknowledges these complexities. Here’s how to do that:
1. Embrace Multiple Standards with Smart Translation Layers
Instead of mandating a single data standard, leading systems now implement translation layers that convert between multiple standards dynamically. For example, a healthcare integration engine can accept HL7 v2 messages from a lab system and translate them into FHIR resources for an EHR.
This approach allows disparate systems to “speak their own language” while still sharing meaningful data, greatly increasing connectivity options.
2. Prioritize Use Case–Driven Interoperability
Not every data exchange requires full standardization. Instead, focusing on high-value use cases—such as medication reconciliation, immunization records sharing, or emergency care data—can deliver tangible benefits faster.
By targeting interoperability goals to specific clinical or operational workflows, organizations can simplify processes and achieve a measurable impact. This also boosts user buy-in by solving real pain points.
3. Leverage APIs and Modular Architectures
Modern interoperable healthcare solutions like AERIS increasingly rely on APIs (Application Programming Interfaces) to facilitate modular and scalable integration. APIs provide standardized access points for different software components, enabling flexible connections without extensive rewrites.
For example, healthcare platforms adopting FHIR-based APIs can allow third-party apps to access patient data securely, expanding functionality and innovation.
4. Promote Collaborative Governance and Stakeholder Engagement
Successful interoperability demands cooperation among all stakeholders—providers, payers, vendors, and regulators. Therefore, establishing governance frameworks that define data-sharing policies, responsibilities, and compliance requirements builds trust and reduces friction.
Engaging end-users such as clinicians and patients early in design also ensures the interoperability solution aligns with their needs.
5. Invest in Scalable Infrastructure and Security
Interoperable healthcare solutions like AERIS can accommodate increasing data volumes and users over time. Cloud computing and edge technologies offer scalable infrastructure to handle this growth while maintaining availability.
Also, the platform’s security measures, such as encryption, role-based access, and audit trails, protect sensitive health data without impeding workflow.
Patient-Centered Interoperability
True interoperability doesn’t just benefit providers—it also empowers patients by granting them control over their health information. Patient portals, personal health records, and mobile apps connected via interoperable systems allow individuals to access, share, and contribute to their own data.
This shift promotes transparency, engagement, and personalized care. Moreover, it supports emerging models like value-based care, which rely on comprehensive, patient-centric data.
Overcoming Interoperability Challenges
Crafting interoperable healthcare systems demands thoughtful design that respects the complexity and diversity of healthcare environments. Here are some final points to consider:
- Flexibility is crucial: Allow systems to communicate across different standards, formats, and technologies.
- Focus on practical use cases: Start interoperability efforts with workflows that provide immediate clinical or operational benefit.
- Involve all stakeholders: Collaboration among healthcare providers, IT vendors, policymakers, and patients builds sustainable ecosystems.
- Leverage modern tech: APIs, cloud infrastructure, and AI enhance integration capabilities.
- Keep security front and center: Protecting patient privacy while facilitating data flow requires robust, adaptable safeguards.
Unlocking Seamless Data Exchange with AERIS
In the quest to build truly interoperable healthcare systems, having a platform that adapts to diverse data standards and seamlessly connects disparate systems is a game changer. AERIS stands out as a cutting-edge adaptive exchange and interoperability platform designed specifically to address the complexities of healthcare data exchange.
Unlike rigid one-size-fits-all solutions, AERIS offers flexibility by supporting multiple healthcare data standards—including HL7, FHIR, and others—while intelligently transforming and routing information to where it’s needed most. This adaptability allows healthcare providers, payers, and technology vendors to connect smoothly regardless of their existing systems or infrastructure.
With AERIS powering your healthcare system, unlocking real-time insights and seamless communication becomes a reality—driving better patient outcomes, operational efficiency, and innovation. Discover how AERIS can transform your healthcare data exchange today.
FAQs
1. Which data standards support interoperable healthcare systems?
Standards like HL7, FHIR, and DICOM are widely used to structure and exchange healthcare information within interoperable systems.
2. How do interoperable healthcare systems improve patient care?
They provide clinicians with real-time access to comprehensive patient information, reducing errors, avoiding duplicate tests, and supporting timely treatment decisions.
3. Can interoperable healthcare systems work with existing legacy software?
Yes, modern interoperable systems use translation layers and APIs to connect legacy software with newer platforms, facilitating gradual integration.
4. What role do APIs play in interoperable healthcare systems?
APIs act as standardized interfaces, allowing different software applications to communicate and exchange data efficiently within interoperable healthcare systems.
5. How do interoperable healthcare systems support patient engagement?
By enabling patient portals and apps to access and share health data securely, they empower patients to take an active role in managing their health.
6. What are interoperable healthcare systems?
Interoperable healthcare systems enable seamless sharing and use of health data across different providers and platforms, improving care coordination and patient outcomes.