Revenue cycle performance impacts the entire healthcare ecosystem. Accurate documentation, correct coding, and timely reimbursements are critical components of a provider’s financial health. Yet, frequent billing errors, claim denials, and compliance issues challenge even the most efficient medical teams. These inconsistencies threaten revenue flow and strain patient trust. Therefore, a system that ensures transparency, accuracy, and alignment between clinical care and billing has become essential. Revenue integrity in healthcare addresses these gaps, reinforcing the foundation of financial operations.
In fact, improved revenue integrity leads to fewer audit risks, faster payments, and better patient outcomes. As the demand for value-based care rises, hospitals must adopt smarter revenue practices. Strengthening hospital revenue cycle management with integrated systems and data-driven strategies is no longer optional—it’s vital. The shift toward automated, compliant, and collaborative processes marks a new era in the healthcare revenue cycle, enabling providers to focus on what matters most: delivering exceptional care
In this blog, we’ll break down revenue integrity in healthcare, its purpose, challenges and best practices.
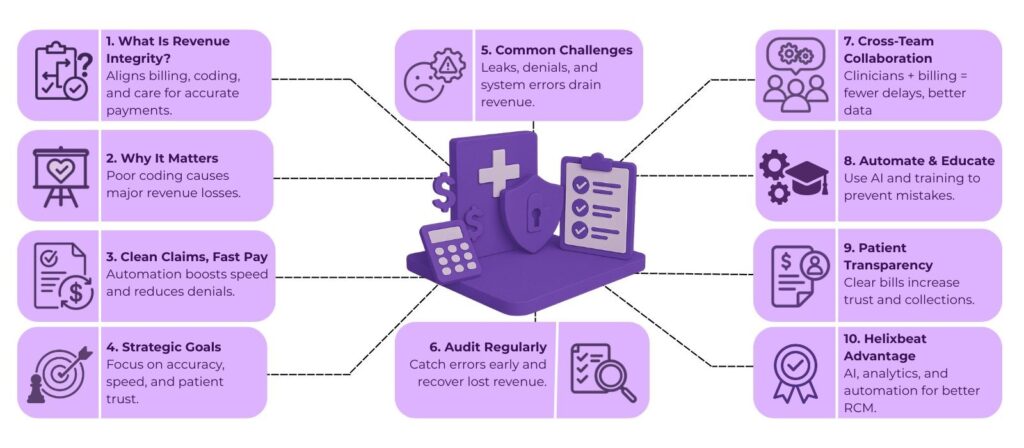
Table of Contents
What is Revenue Integrity in Healthcare?
Revenue integrity in healthcare refers to the coordinated efforts of clinical, financial, and operational teams to ensure accurate documentation, correct coding, and compliant billing for services rendered. The primary aim is to prevent revenue leakage, eliminate billing errors, and maintain regulatory compliance—ultimately optimizing the hospital revenue cycle management process.
The process encompasses the following core functions:
- Documentation: Complete and accurate clinical records that support services billed.
- Coding: Assigning appropriate CPT, ICD-10, and HCPCS codes to ensure correct reimbursement.
- Billing: Submitting claims accurately and on time to avoid denials and delays.
- Compliance: Adhering to healthcare regulations such as HIPAA or payer rules.
By prioritizing revenue integrity in healthcare systems, organizations can reduce costly rework, avoid penalties, and preserve patient trust—all while improving their bottom line.
Key Takeaways (with Statistics):
- 40% of healthcare providers experience revenue leakage due to poor documentation and coding errors.
- 60% of denied claims are recoverable—but only 35% are ever reworked, leading to massive losses.
- $3.5B in annual losses occur from missed or inaccurate charge capture in U.S. hospitals.
- Providers who implement automated RCM solutions like Helixbeat see a 30–50% reduction in claim denials.
- Hospitals that invest in revenue integrity programs report a 20–25% boost in net revenue within the first year.
- Transparent billing practices increase patient collections by over 35%, improving satisfaction and trust.
Strategic Goals for Achieving Revenue Integrity
Hospitals and healthcare providers must develop clear strategic goals to guide revenue integrity initiatives. These objectives are essential to align every stakeholder’s effort towards a common outcome: sustainable revenue without compromising care quality.
1. Enhance Operational Efficiency
Smooth workflows minimize delays in coding, billing, and claims management. Automation and streamlined procedures help reduce bottlenecks in the healthcare revenue cycle.
2. Strengthen Financial Performance
Maximizing revenue capture by accurately billing for every service provided ensures a steady financial stream and supports continued investment in patient care.
3. Minimize Compliance Risks
By following evolving regulations, healthcare providers can mitigate audit risks, avoid fines, and ensure trustworthy relationships with payers and patients.
4. Improve Patient Satisfaction
Transparent and error-free billing reduces patient confusion and disputes, boosting their overall experience and confidence in your healthcare facility.
5. Promote Organisational Accountability
Creating a culture where revenue cycle activities are carefully monitored and accountable empowers every department to maintain high standards.
With these strategic goals in place, providers can achieve stronger revenue integrity in healthcare and elevate the overall performance of the hospital revenue cycle management process.
Addressing Common Revenue Integrity Challenges
Despite its importance, revenue integrity in healthcare faces several obstacles that can hinder success if not properly managed.
1. Revenue Leakage
Even minor coding or documentation errors can snowball into significant revenue losses. Regular audits and training can prevent unnoticed discrepancies.
2. Inaccurate Charge Capture
Missed or incorrect charges, often due to manual processes or system issues, can result in substantial underpayments or claim denials.
3. Incomplete Documentation
If medical records do not support billed services, claims may be denied. This emphasizes the need for clinician education and EMR optimization.
4. Insurance Verification Errors
Failure to verify patient eligibility results in rejected claims or delayed payments, affecting cash flow and staff productivity.
5. Staffing Shortages
Understaffed RCM teams may struggle to maintain quality and speed, resulting in more denials and delayed reimbursements.
6. Changing Regulatory Landscape
Frequent changes in payer rules, coding standards, and federal regulations demand continuous staff training and workflow updates.
7. Inconsistent Processes
Departments with varying procedures may face misalignment, leading to inefficiencies and missed revenue opportunities.
Tackling these challenges is crucial for achieving true revenue integrity in healthcare, and innovative solutions are required to stay ahead of these problems.
Best Practice for Ongoing Optimization of Revenue Integrity
1. Regular Process Audits
Regularly reviewing and auditing billing and coding processes helps healthcare organizations catch inefficiencies, spot discrepancies, and ensure alignment with compliance standards.
Example: A hospital performs quarterly audits on its cardiology department’s billing practices and discovers that EKGs were often coded incorrectly, leading to underpayments. By correcting these errors and retraining staff, the department recovered over $50,000 in lost revenue in just six months.
2. Foster Interdepartmental Collaboration
Encouraging consistent communication and collaboration between departments like clinical care, billing, coding, and compliance reduces silos, enhances data accuracy, and speeds up the revenue cycle.
Example: At a multi-specialty hospital, clinicians started holding monthly meetings with coders and billing staff. As a result, they clarified documentation expectations, reduced the number of claim reworks by 35%, and shortened the average time to payment.
3. Invest in Automation
Automation tools in Revenue Cycle Management (RCM) streamline repetitive tasks like data entry, coding suggestions, and eligibility checks—leading to faster turnaround and fewer errors.
Example: A health system deployed an AI-driven coding platform that suggested the most accurate CPT and ICD-10 codes based on EMR notes. This cut manual coding time in half and reduced claim denials due to coding errors by 40%.
4. Provide Staff Education
What it means: Continuous education on evolving coding standards (like ICD-11 or payer-specific rules) and compliance helps maintain accuracy, minimize denials, and improve claim acceptance rates.
Example: A billing team at a regional clinic attended quarterly webinars on payer updates and ICD-10 changes. After implementing lessons learned, their clean claim rate improved from 82% to 94% within two quarters.
5. Transparency with Patients
Clear and upfront communication with patients about billing, insurance benefits, and out-of-pocket costs increases patient trust and reduces billing disputes.
Example: A hospital implemented pre-visit cost estimations and provided patients with a breakdown of expected charges. Patient satisfaction scores improved by 20%, and collections at the time of service increased by 30%.
6. Strong Denial Management
A robust denial management strategy involves identifying root causes, automating appeal submissions, and continuously tracking outcomes to recover revenue efficiently.
Example: One facility centralized its denial tracking and noticed a trend of missing authorization for MRI procedures. They implemented an automated pre-authorization system, reducing denials by 50% and improving cash flow
7. Use Analytics for Insights
Real-time dashboards and analytics tools help organizations monitor key performance indicators (KPIs) like denial rate, average days in A/R, and first-pass claim acceptance—guiding data-backed decisions.
Example: A health network utilized a business intelligence dashboard to track underperforming service lines. It revealed that their orthopedics department had a 22% denial rate due to documentation gaps. After targeted intervention, denial rates dropped to 10% and revenue increased by 15%.
How Helixbeat Helps You Strengthen Revenue Integrity
At Helixbeat, we understand that maintaining revenue integrity in healthcare is not a one-time project—it’s an ongoing commitment. Our end-to-end RCM solutions are designed to help you optimize every stage of the hospital revenue cycle management process.
Here’s how Helixbeat supports your revenue integrity goals:
- Automated Charge Capture: Our systems ensure all billable services are identified and recorded, minimizing missed charges.
- AI-Driven Coding Assistance: Reduce human error and coding discrepancies with our AI-powered suggestions and validations.
- Eligibility Verification Tools: Real-time insurance verification reduces claim denials and accelerates reimbursement.
- Analytics Dashboard: Get deep visibility into key metrics that impact your healthcare revenue cycle and take action proactively.
- Compliance Monitoring: Stay updated with the latest regulatory changes and ensure your billing practices are audit-ready.
- Denial Management Workflow: Our robust appeal management system ensures denied claims are quickly and accurately resolved.
With Helixbeat, you gain a dedicated partner focused on elevating the accuracy, transparency, and efficiency of your revenue processes—so you can focus on delivering exceptional care
Final thoughts
As the healthcare industry continues to evolve, ensuring revenue integrity in healthcare becomes more crucial than ever. With rising patient financial responsibility, stringent compliance requirements, and increasing administrative complexities, hospitals must adopt proactive strategies that align financial performance with high-quality care.
By understanding its purpose, recognizing common challenges, and applying best practices, your organization can build a resilient and compliant healthcare revenue cycle.
Partnering with experts like Helixbeat can make all the difference in achieving consistent, optimized, and sustainable hospital revenue cycle management.
Let us help you secure every earned dollar—accurately, efficiently, and compliantly.
Frequently asked questions
1. What are some best practices for managing the revenue cycle in a healthcare facility?
Regular audits, team collaboration, automation, staff training, patient transparency, denial management, and data analytics.
2. What is the principle of integrity in healthcare?
Acting with honesty, ethics, and transparency in care delivery, billing, and documentation.
3. How can healthcare organizations optimize their revenue cycle management (RCM)?
By using automation, tracking KPIs, educating staff, reducing denials, and improving patient access and billing clarity.
4. Why is denial management crucial for revenue cycle performance?
It helps recover lost revenue, reduce errors, and improve clean claim rates.
5. How does patient transparency impact revenue cycle outcomes?
It builds trust, improves collections, and reduces billing confusion.
6. What role does technology play in modern revenue cycle management?
Technology streamlines workflows, reduces errors, and enhances billing and data insights.