The healthcare industry is experiencing a massive shift. For decades, healthcare providers, payers, and patients have operated within fragmented systems—characterized by disconnected technologies, isolated data, and siloed communication channels. This fragmentation has created hurdles in delivering seamless, efficient, and patient-centered care. The good news? However, healthcare interoperability is rapidly changing things, and patient care is becoming more connected.
In this blog, we’ll explore what healthcare interoperability is, why it’s important, how its standards are shaping the future, and how new software and platforms are making this big change happen.
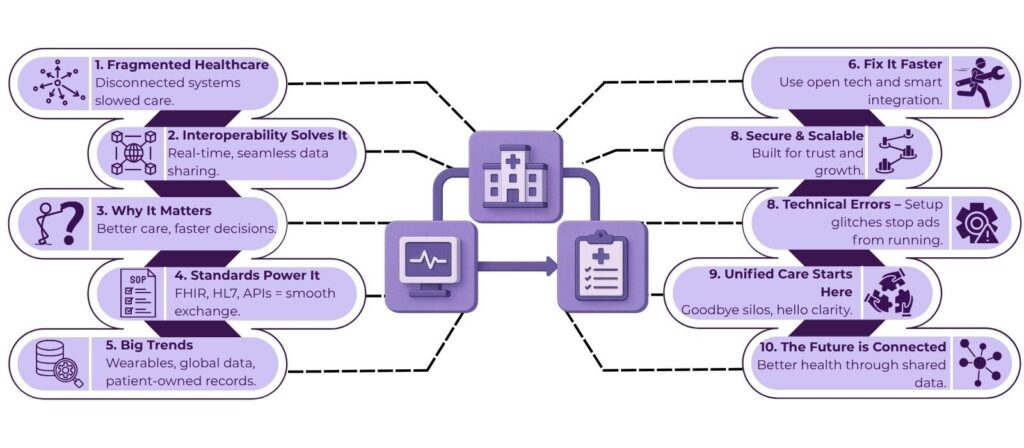
Table of Contents
What is Healthcare Interoperability?
Healthcare interoperability refers to the ability of different health information systems, devices, and applications to access, exchange, interpret, and use data cohesively across organizational boundaries. When systems “talk” to each other effectively, they support comprehensive, coordinated care by sharing accurate, timely, and actionable patient information.
Think of it as building bridges between isolated islands of data, turning them into a connected archipelago where care providers have a full view of a patient’s health journey. This connectivity reduces redundancies, speeds decision-making, and improves patient outcomes.
The Problem with Fragmented Healthcare Systems
Before interoperability gained prominence, healthcare systems were often characterized by:
- Isolated Data Silos: Hospitals, clinics, labs, pharmacies, and insurers used different software with incompatible data formats, which prevented seamless data sharing.
- Manual Data Exchange: Fax machines, emails, and paper records were common tools for transferring information, but they were prone to delays, errors, and lost records.
- Inconsistent Patient Records: Without unified records, clinicians often lacked access to the complete medical history, which led to misdiagnoses or unnecessary repeat tests.
- Administrative Inefficiencies: Billing, claims processing, and care coordination became slow and cumbersome due to fragmented information.
- Poor Patient Experience: Patients had to repeat medical histories, carry physical records, or face delays in care.
This fragmentation created inefficiencies and gaps, sometimes with serious consequences for patient safety and healthcare costs.
Why Healthcare Interoperability Matters Today
The rise of digital health technologies, electronic health records (EHRs), wearable devices, telemedicine, and patient portals has exponentially increased the volume and variety of healthcare data. Without interoperability, these advances risk becoming isolated innovations rather than integrated solutions. However, healthcare interoperability helps by:
- Improving Clinical Decision-Making: Real-time access to comprehensive patient data, including lab results, medication histories, and imaging, allows providers to make informed decisions.
- Enhancing Care Coordination: Specialists, primary care physicians, and care teams can collaborate efficiently by sharing patient updates instantly.
- Reducing Costs: By eliminating duplicate tests and minimizing errors, interoperability lowers unnecessary healthcare spending.
- Boosting Patient Engagement: Patients get easier access to their health information, empowering them to participate actively in their care.
- Supporting Public Health Efforts: Aggregated data enables timely tracking of disease outbreaks, vaccination rates, and population health trends.
How Interoperability Standards in Healthcare Make Connectivity Possible
Standards are the foundation of any interoperable system. Without agreed-upon formats, protocols, and rules, data exchange would be chaotic and unreliable. Some widely adopted interoperability standards in healthcare include:
1. HL7 (Health Level Seven)
HL7 is a set of international standards for transferring clinical and administrative data between software applications. Its versions include HL7 v2 (widely used for messaging) and HL7 v3 (more structured but less widely adopted).
2. FHIR (Fast Healthcare Interoperability Resources)
FHIR, developed by HL7 International, is a modern, web-based standard designed to simplify data exchange using RESTful APIs, JSON, and XML formats. It supports granular, real-time access to healthcare data and is rapidly becoming the backbone of healthcare interoperability platforms.
3. DICOM (Digital Imaging and Communications in Medicine)
DICOM is the standard for handling, storing, and transmitting medical imaging information such as X-rays and MRIs.
4. CDA (Clinical Document Architecture)
CDA specifies the structure and semantics of clinical documents to facilitate document exchange.
5. SNOMED CT and LOINC
These are standardized vocabularies for clinical terms and laboratory observations, respectively, to ensure consistent interpretation of data.
Where Healthcare Interoperability is Heading
As healthcare systems globally embrace interoperability, several exciting trends are emerging:
1. Nationwide Health Information Exchanges (HIEs)
Many countries are establishing HIEs—centralized platforms that connect providers across regions—to facilitate seamless data sharing.
2. Patient-Controlled Health Records
Initiatives are pushing toward giving patients ownership of their health data through personal health records (PHRs) and mobile apps.
3. Integration of Wearables and IoT Devices
Data from fitness trackers, smartwatches, and home monitoring devices are increasingly integrated into clinical workflows for continuous, real-time health monitoring.
4. Precision Medicine and Genomics
By linking clinical data with genetic details, interoperable systems help doctors customize treatments for each patient.
5. Cross-Border Healthcare Data Sharing
As medical tourism grows and pandemics highlight global health interdependence, interoperability across countries becomes more important.
How Healthcare Organizations Can Accelerate Interoperability
To capitalize on the benefits of healthcare interoperability, organizations can take these strategic steps:
- Adopt Open Standards: Choose vendors and platforms that support widely accepted interoperability standards like FHIR.
- Invest in Integration Platforms: Use middleware and APIs to connect disparate systems effectively.
- Focus on Data Governance: Establish clear policies on data privacy, consent, and quality management.
- Engage Stakeholders: Involve clinicians, IT staff, patients, and partners in designing interoperable workflows.
- Prioritize Training and Change Management: Equip teams with the knowledge and tools to leverage interoperable technologies.
AERIS: Powering Real-Time Healthcare Data Exchange with FHIR
As the healthcare industry moves toward greater interoperability, having the right technology partner is necessary. AERIS by Helixbeat stands out as a cutting-edge FHIR-based platform designed to facilitate real-time, seamless data exchange between diverse healthcare systems.
Built on the latest HL7 FHIR standards, AERIS enables healthcare providers, labs, pharmacies, and other stakeholders to share and access critical patient data instantly and securely. This real-time interoperability helps eliminate data silos and accelerates clinical decision-making, supporting a truly connected care environment.
Key features of AERIS include:
- Fast and Reliable Data Exchange: Enables instant communication between heterogeneous systems, improving care coordination and patient outcomes.
- Standards-Driven Architecture: Fully compliant with FHIR and other interoperability protocols to maximize compatibility and future-proof your infrastructure.
- Secure and Compliant: Incorporates robust security measures and privacy controls aligned with healthcare regulations.
- Scalable and Flexible: Easily integrates with existing IT landscapes and scales with your organization.
By choosing AERIS, healthcare organizations can break down barriers created by fragmented systems and unlock the full potential of connected care.
Final Thoughts
The rise of healthcare interoperability marks a fundamental shift from isolated, fragmented systems toward a connected, patient-centered care ecosystem. While challenges remain, ongoing advancements in standards, technology, and collaboration are paving the way for truly integrated healthcare.
The journey from fragmentation to connection is not just a technical evolution—it’s a commitment to better health outcomes for all. Discover how AERIS can transform your data exchange workflows and drive the future of healthcare interoperability.
FAQs
1. Can healthcare interoperability help patients manage their own health data?
Yes, interoperability empowers patients by giving them easier access to their medical records and facilitating better engagement with their care plans.
2. What role does technology play in advancing healthcare interoperability?
Modern technologies like APIs and cloud computing support real-time, secure, and scalable data exchange, which is necessary for interoperability.
3. How does healthcare interoperability affect healthcare costs?
By minimizing redundant tests and administrative tasks, healthcare interoperability can help reduce unnecessary expenses and improve overall efficiency.
4. Is healthcare interoperability the same as data integration?
While related, healthcare interoperability emphasizes not only data sharing but also preserving meaning and usability across different systems, beyond just integration.
5. What steps can healthcare organizations take to achieve better healthcare interoperability?
Organizations should adopt open standards, invest in integration platforms, implement strong data governance, and boost collaboration among all stakeholders.