Today, healthcare interoperability serves as a foundation for efficiently exchanging data between systems, providers, and patients. It means seamlessly sharing and using electronic health data across various platforms to improve patient outcomes and simplify operations. However, with complex regulatory environments and fast-moving technology, organizations really need a clear strategy to navigate everything.
To help you succeed, this blog outlines a complete strategy for healthcare interoperability, backed by established standards and emerging trends.
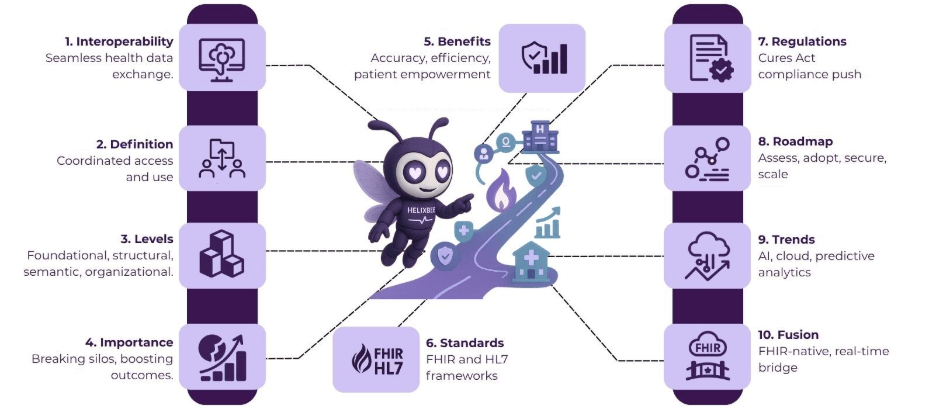
Table of Contents
What is Healthcare Interoperability?
Healthcare interoperability is the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner. Simply put, it gives you quick and secure access to electronic health data, making it possible to achieve better health outcomes. The Health Information Management Systems Society (HIMSS) describes it as the individuals, systems, and processes that share and access every type of health information, including data created by patients.
There are four levels of healthcare interoperability: foundational, where data moves from one system to another without interpretation; structural, involving standardized formats; semantic, enabling systems to interpret shared data; and organizational, which incorporates governance and policy for seamless cross-entity exchange. Achieving higher levels requires alignment of technology, standards, and workflows, ultimately supporting comprehensive care delivery.
The Importance of Healthcare Interoperability
Healthcare interoperability plays a key role in modernizing medical practices by breaking down data silos. With the increase of electronic health records (EHRs), wearable devices, and telehealth platforms, the need for integrated data flows has intensified. Moreover, regulations like the 21st Century Cures Act emphasize this by mandating measures to advance data exchange and prohibit information blocking, encouraging a more connected ecosystem.
This interconnectedness supports value-based care models, where providers focus on outcomes rather than volume. By enabling real-time data access, healthcare interoperability reduces redundancies, minimizes errors, and empowers patients to take control over their information. As global health systems face increasing demands, prioritizing interoperability will become critical for sustainable progress.
Key Benefits of Achieving Healthcare Interoperability
Healthcare interoperability brings many benefits that change both patient care and operational efficiency. Here are a few:
- Improved Patient Outcomes: When data sharing is seamless, providers can access complete medical histories, leading directly to more accurate diagnoses and personalized treatments.
- Enhanced Efficiency and Cost Savings: By eliminating duplicate tests and paperwork, organizations save time and resources. Even studies indicate that effective interoperability can lower administrative costs significantly.
- Better Care Coordination: Interoperable systems facilitate collaboration among multidisciplinary teams, supporting transitions between primary care, hospitals, and long-term facilities.
- Empowered Patients: Patients gain access to their data through portals and apps, promoting engagement and informed decision-making.
- Data-Driven Insights: Aggregated data enables population health management, predictive analytics, and research advancements.
These benefits collectively contribute to a more resilient healthcare system, capable of responding to public health challenges like pandemics.
Standards and Regulations for Healthcare Interoperability
Standards form the backbone of healthcare interoperability. Health Level Seven International (HL7) provides frameworks like Fast Healthcare Interoperability Resources (FHIR), an API-focused standard for quick and efficient data exchange, including clinical and administrative information. FHIR Release 4.0.1, maintained by HL7, defines how healthcare information moves electronically.
Besides, regulations drive adoption. The final rule of the 21st Century Cures Act outlines the requirements for health IT certification, boosting interoperability while addressing information blocking. The Centers for Medicare & Medicaid Services (CMS) Interoperability and Patient Access Final Rule liberates patient data, using authority to enhance access through APIs. These guidelines set the stage for compliant, effective systems.
A Step-by-Step Strategic Roadmap for Healthcare Interoperability Success
To achieve healthcare interoperability, organizations should follow a structured roadmap. Here’s a general idea:
- Assess Current State: Evaluate existing systems, data flows, and gaps. Conduct audits to identify silos and compliance issues.
- Define Objectives and Governance: Establish clear goals, such as improving patient access or reducing costs. Form governance committees to oversee policies and stakeholder alignment.
- Adopt Standards and Technologies: Implement FHIR and HL7 protocols. Integrate APIs and cloud-based platforms for scalable exchange.
- Build Secure Infrastructure: Deploy encryption, authentication, and monitoring tools to protect data during transmission.
- Train Staff and Foster Culture: Provide education on new systems and encourage a collaborative mindset among teams.
- Test and Iterate: Pilot integrations, gather feedback, and refine processes based on performance metrics.
- Monitor and Scale: Continuously track outcomes, update systems, and expand to include partners like payers and pharmacies.
This roadmap, inspired by nationwide frameworks, promotes incremental progress toward full interoperability.
Future Trends in Healthcare Interoperability
Looking ahead, healthcare interoperability will evolve with technologies like artificial intelligence (AI). With AI, providers can analyze data better, predict needs, and automate exchanges. Thanks to cloud computing and advanced APIs like FHIR, patient-centric models are becoming the standard.
Meanwhile, regulatory pushes will accelerate adoption, with trends focusing on fraud prevention and enhanced privacy. These innovations promise a more interconnected, efficient future.
FUSION: Supercharge Your Healthcare Solutions with FHIR APIs
Built with RESTful APIs, FUSION is a FHIR server created to deliver easier, faster, and more accurate data exchange.
FUSION stores patient data in FHIR format, which is the global standard for healthcare data. This enables different apps, hospitals, and systems to communicate with each other and share critical health information in real-time.
What sets FUSION apart is that it also stores medical coding systems like SNOMED CT, LOINC, and ICD. This keeps all data consistent, accurate, and ready for clinical use, reporting, and analytics.
Key features of FUSION include
- FHIR-native architecture
- Plug-and-play APIs for rapid deployment
- Real-time data sharing across multiple endpoints
- Strong security controls that meet compliance standards
- Support for both structured and unstructured data
Whether a hospital wants to exchange records with external labs or enable app-based clinical tools, FUSION acts as the smart bridge, without needing to replace existing infrastructure.
Final Thoughts
Healthcare interoperability transforms care by delivering better results through strategic planning and technological adoption. By following this roadmap, organizations can navigate challenges and harness benefits, ultimately advancing health systems.
Discover how FUSION, with its FHIR-native architecture, can transform your healthcare systems today.
FAQs
1. Why is healthcare interoperability important?
Interoperability helps modernize healthcare by breaking down data silos, improving access to real-time patient data, and supporting better care coordination across providers.
2. What are the key benefits of healthcare interoperability?
It improves patient outcomes, enhances operational efficiency, lowers costs, fosters better care coordination, empowers patients, and provides valuable data-driven insights.
3. How does healthcare interoperability impact patient care?
By allowing seamless data sharing, healthcare interoperability helps providers access complete medical histories, leading to more accurate diagnoses and personalized treatment plans.
4. What standards are used in healthcare interoperability?
Standards like HL7 and Fast Healthcare Interoperability Resources (FHIR) are used to structure data exchange, enabling systems to share clinical and administrative information efficiently.
5. What is FUSION, and how does it help with interoperability?
FUSION is a FHIR server that stores patient data in FHIR format, enabling real-time data sharing across systems and ensuring consistent, accurate information for clinical use.