Today, sharing patient information quickly and accurately can make all the difference in care. Imagine a doctor in one clinic pulling up your complete medical history from another hospital without hassle. That’s the power of interoperability in health information systems.
In this blog, we’ll discuss the four main types of interoperability in healthcare: foundational, structural, semantic, and organizational. We’ll break them down in simple terms, explore their roles, and see how they work together to improve patient outcomes.
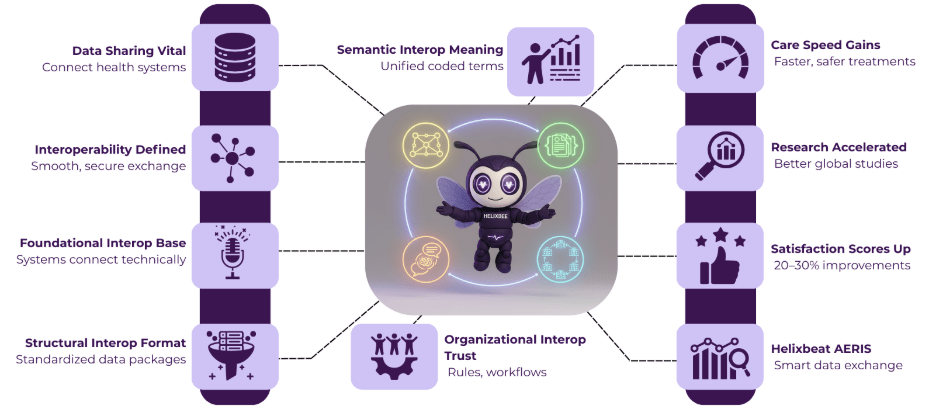
Table of Contents
What Is Interoperability in Health Information Systems?
In short, interoperability in health information systems means different technologies, apps, and devices can communicate and exchange data smoothly. Think of it like people speaking the same language—no lost-in-translation moments. In healthcare, this involves electronic health records (EHRs), lab results, imaging tools, etc., all talking to each other.
Why does this matter? When systems don’t connect well, doctors waste time hunting for info, patients face delays, and errors creep in. Good interoperability in health information systems mitigates these risks, speeds up decision-making, and reduces costs.
The Four Types of Interoperability in Healthcare
Let’s unpack each type. We’ll look at what it does, real-world examples, and its impact on daily healthcare tasks.
Foundational Interoperability
Foundational interoperability is the groundwork. It focuses on the technical ability of systems to recognize and connect, much like plugging in a USB cable that fits any device. This type handles the “can they connect?” question without worrying about what the data means yet.
In practice, this involves standard protocols like TCP/IP, which power the internet. In healthcare, it might mean a hospital’s server pinging a clinic’s system to start a data transfer. Without this base layer, nothing else works—it’s the on-switch for interoperability in health information systems.
Structural Interoperability
Once connected, systems need a common way to package data. That’s where structural interoperability steps in. It deals with how information is organized and sent, like agreeing on envelope sizes for letters so they fit through mail slots.
This type uses standards such as HL7 or FHIR (Fast Healthcare Interoperability Resources), which define data structures. For example, a patient’s blood pressure reading is now put into a consistent format—numbers, units, and a timestamp all in one neat bundle. That means no more trying to decipher scribbles or mismatched files.
In a busy ER, structural interoperability really shines when an ambulance app sends ECG results straight to the team’s screens in real-time. It cuts setup time from minutes to seconds. However, not all systems use the same standards. As more tools adopt FHIR, this type strengthens the backbone of interoperability in health information systems.
Semantic Interoperability
Now, data isn’t just formatted— it has to mean the same thing everywhere. Semantic interoperability helps solve the interpretation problem—so a “high blood sugar” note means the same thing to a doctor in the U.S. as it does to one in Europe.
This relies on coded terminologies: SNOMED CT for diagnoses, LOINC for lab tests, or RxNorm for medications. A fever might code as “SNOMED: 386661006,” so software knows it’s the same condition, not a vague symptom.
Picture a patient switching oncologists mid-treatment. Semantic tools let the new doc see exact chemo details, which helps avoid mix-ups that could harm health. In global health crises, like pandemics, this type unifies outbreak reports worldwide. Therefore, semantic layers upgrade interoperability in health information systems from mere transfer to true understanding.
Organizational Interoperability
The final piece is organizational interoperability, which goes beyond tech to human and process alignment. It covers agreements, trust rules, and workflows that govern data sharing—like a team’s playbook for smooth plays.
This involves consent forms, adherence to privacy laws (such as HIPAA), and partnerships between healthcare providers. A hospital might partner with a pharmacy chain, establishing rules for who has access to what and when.
For chronic illness management, an organizational setup enables a primary care doctor, specialist, and home monitor to share updates via agreed-upon channels.
Therefore, organizational interoperability builds trust, which is vital in sensitive fields like mental health. It ties everything together, turning isolated systems into a collaborative network for interoperability in health information systems.
Benefits of Strong Interoperability in Health Information Systems
When these four types click, the wins pile up. Patients get faster, more personalized care—think allergy alerts popping up instantly. Providers save hours on paperwork and focus on healing instead. Payers see fewer billing errors and over-testing.
On a bigger scale, research accelerates. For example, aggregated data from connected systems can inform studies on disease patterns and speed up vaccine development. Rural areas gain urban-level expertise through telehealth links. Even studies show that interoperability in health information systems boosts satisfaction scores by 20-30% for both patients and staff.
AERIS: Streamlining Data for Smarter Care
AERIS by Helixbeat is a state-of-the-art healthcare interoperability solution designed to make data exchange across systems smoother and more efficient. It effortlessly brings together patient information from various sources, helping healthcare providers deliver more accurate and timely care.
With HL7 and FHIR, AERIS facilitates secure, real-time data sharing across platforms, improving decision-making and operational efficiency. As a result, healthcare organizations can manage patient records with ease, reduce administrative tasks, and foster better collaboration—all while staying in line with HIPAA regulations.
Final Thoughts
Interoperability in health information systems isn’t a buzzword—it’s the glue holding modern medicine together. From foundational links to organizational teamwork, each type plays a key role in creating a web where data flows freely and safely.
As we move forward, embracing these layers will transform care. Patients live better, providers work smarter, and communities stay healthier. Unlock the potential of HL7 and FHIR with AERIS and turn data into meaningful insights! Contact us today.
FAQs
1. What is interoperability in health information systems?
Interoperability refers to the ability of different healthcare technologies, devices, and applications to exchange and understand data smoothly, improving decision-making and care.
2. What are the four types of interoperability in healthcare?
The four types are foundational, structural, semantic, and organizational interoperability, each playing a unique role in improving how health data is exchanged and understood.
3. How does AERIS facilitate healthcare interoperability?
AERIS uses HL7 and FHIR standards to facilitate seamless, real-time data sharing across systems, helping healthcare providers make informed decisions more quickly.
4. What are the benefits of interoperability in healthcare?
Benefits include faster and more personalized care, reduced paperwork, fewer billing errors, better research, and improved satisfaction for both patients and providers.
5. How does AERIS support healthcare organizations?
AERIS streamlines data sharing, reduces administrative burdens, promotes collaboration, and helps healthcare organizations comply with HIPAA regulations while improving operational efficiency.