In an industry as dynamic and intricate as healthcare, administrative efficiency can make or break the financial stability of an organization. From the moment a patient schedules an appointment to the final payment collection, multiple processes and stakeholders are involved. Traditionally, RCM has been labor-intensive and prone to delays, denials, and data entry errors. But automation is rapidly reshaping this landscape.
With the healthcare sector grappling with staffing shortages, rising operational costs, and stricter compliance mandates, automated systems are now pivotal in driving both productivity and profitability.
In this blog, we’ll explore how automation is transforming every stage of RCM, the benefits healthcare providers are already seeing, and what this means for the future of financial operations in hospitals and clinics.
Table of Contents
Revenue Cycle Management: The Basics
Before diving into the impact of automation, it’s helpful to understand what RCM constitutes. Revenue Cycle Management refers to all the administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. It involves several key steps:
- Patient registration
- Insurance verification
- Appointment scheduling
- Medical coding
- Claim submission
- Payment posting
- Denial management
The Need for Automation in RCM
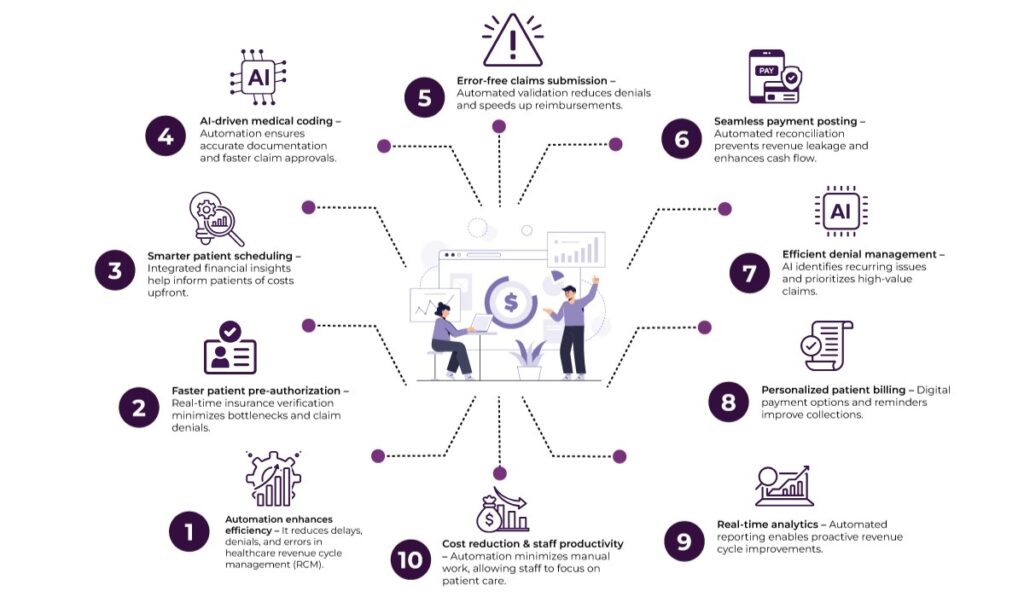
Here’s how automation can help healthcare organizations streamline operations and reduce costly errors:
1. Speeding Up Patient Pre-Authorization and Eligibility Checks
Verifying insurance eligibility and getting pre-authorizations is often one of the biggest bottlenecks in the revenue cycle. Also, manually handling these steps can drag on for hours or even days.
With automated tools, providers can instantly verify a patient’s insurance status by tapping into payer databases in real-time. These tools can also detect potential issues—like coverage lapses or non-covered services—well before the appointment. That gives staff time to resolve problems proactively and reduce the likelihood of claim denials.
2. Smarter Patient Scheduling with Financial Insight
Modern automation platforms integrate financial data with patient scheduling tools. This means front-desk staff can see not only appointment availability but also whether the patient has a high-deductible plan or outstanding balances.
This financial transparency allows for better conversations at the point of service. As a result, patients can be informed of their expected out-of-pocket costs upfront, which leads to more accurate billing and fewer surprises post-treatment.
3. Automated Coding and Documentation Support
Medical coding is a critical part of RCM. Errors here often lead to claim denials or underpayments. Traditional coding processes rely heavily on human input, which can be inconsistent—especially with frequent updates to coding standards like ICD-10 or CPT.
Automation, powered by natural language processing (NLP) and artificial intelligence (AI), can scan clinical notes and suggest accurate codes. These tools reduce the cognitive burden on coders and improve documentation consistency. The result? Faster turnaround times and higher claim approval rates.
4. Streamlined Claims Management and Submission
Submitting claims is one of the most sensitive parts of the revenue cycle. A typo, a missing modifier, or a mismatched code can derail the entire payment process.
Automated RCM systems validate claims before submission, checking for common errors, mismatched data, or policy violations. These pre-checks significantly reduce the volume of denied or rejected claims. Once validated, claims can be submitted electronically to multiple payers simultaneously and fast track the reimbursement timeline.
5. Faster Payment Posting and Reconciliation
Once payments arrive—whether from insurance companies or patients—the next step is to apply them to the appropriate accounts. Doing this manually, especially for high-volume practices, is tedious and ripe for error.
Automated payment posting tools match remittance advice with billed claims and update accounts in real-time. They also handle partial payments and identify discrepancies automatically. This not only accelerates reconciliation but also flags potential revenue leakage, which helps financial teams act quickly.
6. Intelligent Denial Management
Claim denials are inevitable, but how they’re handled makes a big difference in revenue recovery. Manually reviewing and appealing denied claims is time-consuming and often deprioritized due to staffing constraints.
Automation tools can categorize denials, identify recurring patterns, and prioritize high-value claims for rework. Some platforms even auto-correct simple errors and resubmit claims without human intervention. Over time, this data can be used to fine-tune billing practices, which reduces the denial rate altogether.
7. Personalized Patient Billing and Collection
Patients are now the fastest-growing payers in healthcare due to high-deductible health plans and co-pays. Yet, many billing systems still send out generic statements without payment guidance.
Automated patient engagement platforms deliver personalized billing via text, email, or patient portals. These tools can:
- Break down bills into understandable formats
- Offer payment plans based on patient history
- Trigger friendly reminders for overdue balances
- Accept digital payments via multiple channels
This approach not only improves the patient experience but also boosts collection rates and reduces administrative burdens.
8. Real-Time Reporting and Analytics
Without visibility into the performance of the revenue cycle, it’s difficult to pinpoint bottlenecks or forecast revenue. However, traditional reporting methods involve pulling data from siloed systems, which often leads to outdated or incomplete insights.
Automated RCM platforms provide real-time dashboards that offer insights into claim status, denial trends, collection rates, etc. As a result, leaders can make faster, data-driven decisions—whether it’s reallocating staff, adjusting payer strategies, or reworking flawed processes.
9. Enhancing Staff Productivity
Healthcare teams often juggle hundreds of tasks daily, from scheduling to paperwork to follow-ups. Automation lifts this burden.
By offloading repetitive tasks to machines, staff can focus on meaningful work—like assisting patients, resolving complex billing queries, or improving clinical documentation. This not only boosts morale but also improves the accuracy and consistency of RCM processes.
10. Reducing Operational Costs
Every manual touchpoint in the revenue cycle comes with a cost—whether it’s in terms of time, labor, or delayed reimbursements. Automation reduces the need for repetitive manual interventions and cuts down the number of follow-up calls, corrections, and re-submissions. This operational efficiency leads to measurable cost savings.
Challenges and Considerations
Of course, automation isn’t a magic wand. Healthcare providers must choose RCM platforms that integrate well with their existing Electronic Health Record (EHR) systems and workflows. Similarly, training staff, setting up proper data governance, and maintaining compliance with HIPAA and other regulations are necessary.
Moreover, automation should support—not replace—human decision-making. In high-touch industries like healthcare, empathy and judgment still play vital roles in patient communication and financial counseling.
The Future of RCM Is Digital
As the healthcare landscape becomes more complex, financial sustainability depends on how efficiently providers manage their revenue cycles. Healthcare organizations that embrace RCM automation are shifting from reactive to proactive revenue management, from generic to personalized patient engagement, and from burnout to better workflows.
In a world where both patients and payers demand more accuracy, transparency, and speed—automation is the competitive edge healthcare providers need to thrive.
FAQs
1. Why is automation important in RCM?
Automation helps healthcare providers reduce delays, minimize manual errors, and streamline complex processes like insurance verification, claim submission, and denial management.
2. What kind of insights can automated reporting tools offer?
Automated RCM platforms provide real-time dashboards that reveal trends in collections, denials, and claim statuses, helping leadership make quick and informed decisions.
3. Does automation help reduce operational costs?
Yes, by minimizing manual interventions and reducing rework, automation increases efficiency and cuts down on labor and administrative expenses.
4. How does automation personalize patient billing?
Automated billing systems send tailored statements via digital channels, offer custom payment plans, and support multiple payment methods to improve collection outcomes.
5. How is denial management improved through automation?
Automation tools can categorize and prioritize denied claims, detect recurring issues, and even correct and resubmit claims automatically.













