No one enjoys the stress of medical bills. Patients are often left confused by cryptic invoices, while providers juggle delayed payments, denied claims, and administrative overload. It’s exhausting, inefficient, and worst of all, it takes time away from what truly matters—delivering care.
The truth is, outdated systems in Revenue Cycles in Healthcare are holding everyone back. But it doesn’t have to be this way. What if payments were seamless, claims were processed in real time, and patients actually understood what they owed—before walking out the door?
That’s the power of digital transformation. And companies like Helixbeat are making it happen. With smart tools, real-time dashboards, and human-first service, Helixbeat is reimagining healthcare finance from the ground up.
In this blog, we’ll explore how their personalized RCM solutions are not only solving the pain points of today but building a better, faster, and more compassionate system for tomorrow.
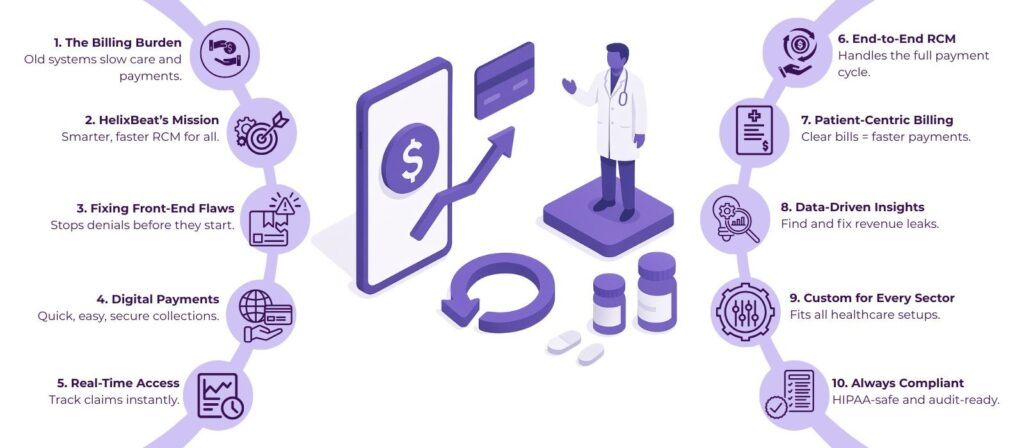
Table of Contents
The Modern Challenges in Revenue Cycles in Healthcare
Healthcare may have made great strides in treatment and technology, but behind the scenes, the financial engine—known as the Revenue Cycle—often still runs on outdated, inefficient systems. Traditional Revenue Cycles in Healthcare are burdened with manual data entry, siloed departments, paper-based billing, delayed reimbursements, and reactive denial management. These gaps create ripple effects that impact not just the bottom line but also patient satisfaction and staff morale.
According to the Medical Group Management Association (MGMA), healthcare providers lose up to 5% of their net revenue due to revenue cycle inefficiencies. Even more alarming is the fact that 90% of claim denials are preventable, yet many organizations continue to rely on fragmented systems and undertrained staff to manage critical billing functions.
These inefficiencies mean more accounts receivable (AR) days, which tie up working capital and delay provider payments. Front-desk staff often juggle multiple tasks, increasing the risk of missed insurance eligibility checks or incorrect patient data entry—two leading causes of claim denials.
Example: Consider a small physician group with limited administrative resources. They routinely face claim denials because of insurance eligibility errors—issues that could easily be caught upfront. For every denied claim, their staff spends hours contacting insurers, revising forms, and resubmitting documentation. That’s time that could’ve been spent on patient engagement, care coordination, or even preventative health initiatives. Instead, they’re stuck in a billing loop.
This is exactly where Helixbeat makes a difference. By automating front-end tasks like insurance verification and leveraging intelligent workflows, Helixbeat minimizes manual errors and prevents denials before they happen. Their system flags issues in real time, ensuring that providers can focus on delivering quality care while the financial side runs smoothly in the background.
Digital Payments: Streamlining the Front-End of Revenue Cycles in Healthcare
Digital payment solutions have emerged as a game-changer in Revenue Cycles in Healthcare. They make it easier for patients to pay bills, help providers collect payments faster, and improve overall financial transparency.
Studies show that 77% of patients prefer digital payment options over traditional billing methods. Moreover, healthcare providers that adopt digital payment systems see a 30% increase in patient collections.
Helixbeat integrates digital payment platforms directly into its RCM services, allowing for real-time patient collections and reduced billing cycles. Whether it’s credit card payments, e-checks, or mobile wallets, Helixbeat’s system ensures seamless transactions that are both HIPAA and PCI-compliant.
Example: A dental practice using Helixbeat saw a 30% improvement in upfront collections after implementing real-time digital payment options at the time of appointment booking. This not only boosted their cash flow but also minimized the follow-up efforts needed for late payments.
Real-Time Access: Empowering Providers and Patients
Real-time access to financial data is crucial for effective decision-making in Revenue Cycles in Healthcare. Helixbeat’s analytics dashboard provides healthcare providers with real-time updates on claim statuses, denials, reimbursements, and financial KPIs.
According to a report by HFMA, organizations that implement real-time access systems reduce claim processing time by up to 45%, leading to faster reimbursements and fewer administrative errors.
Healthcare administrators can instantly track which claims are approved, which are pending, and which require further documentation. This reduces lag in the revenue cycle and empowers organizations to take corrective action immediately.
Example: A mid-sized hospital using Helixbeat’s real-time dashboards reduced their AR days by 18% within the first quarter. This was achieved by proactively addressing pending claims before they became problematic.
End-to-End RCM: Reinventing Revenue Cycles in Healthcare with Helixbeat
What sets Helixbeat apart is its comprehensive, end-to-end approach to managing Revenue Cycles in Healthcare. Their service model covers:
- Patient Registration & Eligibility Verification: Ensures accurate patient intake and real-time insurance checks to prevent claim denials. Organizations that verify insurance in real time reduce denials by up to 60%.
- Medical Coding & Billing: Accurate coding with compliance to ICD-10, CPT, and HCPCS standards. Proper coding increases the likelihood of clean claim submission by 25%.
- Claims Management: End-to-end submission and proactive payer follow-ups. Efficient claim management can improve cash flow by 20%.
- Accounts Receivable (AR) Management: Strategic follow-ups to reduce aging balances. Average industry standard is 40 AR days; Helixbeat clients report reducing this to under 30 days.
- Denials Management: In-depth root cause analysis and appeal handling. Denial recovery success rates improve by up to 35% with Helixbeat.
- Payment Posting: Precise allocation of payments and transparency in reporting. Automated payment posting reduces manual errors by 70%.
- Compliance: HIPAA-compliant processes and regular audits to ensure regulatory integrity. Regular audits lower compliance risks by 50%.
Personalized Financial Care = Better Health Outcomes
When Revenue Cycles in Healthcare are efficient, patients benefit from fewer billing errors, clearer communication, and better financial planning. Helixbeat promotes this personalized financial care approach.
According to a TransUnion Healthcare study, 75% of patients are confused by their medical bills, leading to delayed or missed payments. Clear financial communication increases payment likelihood by 65%.
Example: Behavioral health providers partnered with Helixbeat reported a 40% reduction in patient complaints related to billing. Transparent communication and quick resolution of issues built trust, ultimately leading to higher patient retention and satisfaction.
Data-Driven Decisions in Revenue Cycles in Healthcare
Data is the new currency in healthcare. With Helixbeat’s reporting and analytics, healthcare providers can make strategic decisions to improve collections, reduce denials, and forecast revenue accurately.
Research from Deloitte shows that data-driven revenue cycle strategies improve net collection rates by up to 25%.
Example: An ambulatory surgical center (ASC) leveraged Helixbeat’s monthly financial reports to identify a consistent pattern of underpayments from a specific payer. After initiating a compliance audit, they recovered thousands in missed reimbursements.
Supporting Every Healthcare Vertical
Helixbeat tailors its RCM services to a wide range of healthcare sectors, each with unique needs in Revenue Cycles in Healthcare:
- Hospitals & Health Systems
- Home Health Agencies
- Urgent Care Centers
- Physician Groups
- Dental Clinics
- Behavioral Health Providers
- Ambulatory Surgical Centers (ASCs)
A study from Black Book Market Research indicates that specialized RCM vendors like Helixbeat increase revenue performance by 29% across diversified healthcare verticals.
This versatility ensures that each client gets a solution optimized for their workflow, regulatory environment, and patient demographics.
Compliance Isn’t Optional—It’s Integral
With ever-evolving regulations, staying compliant in Revenue Cycles in Healthcare is critical. Helixbeat’s built-in compliance checks and internal controls ensure your operations remain audit-ready at all times.
According to a PwC report, non-compliance in healthcare billing can cost organizations an average of $1.5 million in fines and lost reimbursements annually.
Regular training, system updates, and audits ensure that clients are never caught off guard by new payer or HIPAA regulations.
The Future of Revenue Cycles in Healthcare
As digital transformation accelerates, the future of Revenue Cycles in Healthcare will be defined by automation, real-time access, and patient-centric financial experiences. Helixbeat is already paving this path, offering a scalable solution that grows with the provider’s needs.
The global RCM market is projected to reach $230 billion by 2030, according to Grand View Research, highlighting the importance of robust, future-ready solutions.
Imagine a future where patients receive their bills within minutes of treatment, pay with a single tap, and providers get reimbursed within days—not weeks. With Helixbeat, that future is already here.
Conclusion
The phrase “Revenue Cycles in Healthcare” is evolving into a dynamic ecosystem that requires expertise, technology, and a patient-first mindset. Helixbeat delivers all three through its personalized, data-driven, and digitally powered RCM services.
From digital payments to real-time dashboards, Helixbeat is revolutionising revenue cycles in Healthcare—making them faster, smarter, and more patient-focused. If you’re ready to transform your financial operations and improve care delivery, it’s time to partner with Helixbeat.
Get a custom consultation today and take the first step toward a healthier revenue cycle.
Our customer also asking
1. What are Revenue Cycles in Healthcare?
Revenue cycles in healthcare refer to the entire financial process—from patient registration to final payment—that healthcare providers use to manage billing and reimbursements.
2. Why are traditional revenue cycles in healthcare inefficient?
They rely on manual processes, outdated billing systems, and delayed reimbursements, leading to denied claims, increased AR days, and administrative burdens.
3. How does Helixbeat improve revenue cycle management?
Helixbeat offers end-to-end RCM solutions with automation, real-time dashboards, digital payments, and personalized service to reduce errors and speed up collections.
4. What are the benefits of digital payments in healthcare?
Digital payments simplify the billing process, improve patient satisfaction, increase upfront collections, and reduce follow-up for late payments.
5. How does real-time access impact healthcare revenue cycles?
Real-time access helps providers track claims, reduce processing times, prevent denials, and make faster, more informed decisions for financial health.
6. Is Helixbeat’s system secure and compliant?
Yes, Helixbeat follows HIPAA standards, conducts regular audits, and uses secure platforms to protect patient and financial data.
7. Which healthcare providers can benefit from Helixbeat?
Helixbeat supports hospitals, physician groups, urgent care centers, ASCs, home health, dental, and behavioral health providers with tailored RCM solutions.














