Did you know that nearly 30% of healthcare claims are rejected due to errors in billing, leading to significant financial losses for healthcare providers? In modern healthcare environment, RCM in medical billing is more important than ever.
However, traditional billing processes are often riddled with inefficiencies, human errors, and delayed payments, which negatively impact cash flow and revenue cycle performance. These challenges not only increase operational costs but also hinder the ability of healthcare providers to deliver quality care.
The solution? Automation in revenue cycle management solutions. By automating key functions within the RCM cycle in medical billing, healthcare providers can significantly reduce errors, accelerate claim processing, and improve overall revenue integrity. Here, we will explore how automation is changing the landscape of RCM in medical billing.
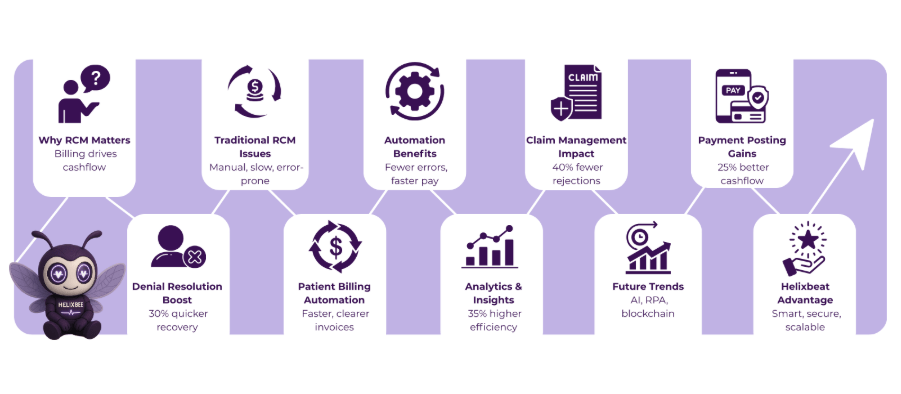
Table of Contents
The Common Challenges in Traditional RCM
Traditional RCM in medical billing is often burdened with inefficiencies and operational hurdles that can severely impact a healthcare provider’s revenue cycle. Below are the key challenges that organizations face when relying on outdated billing systems:
1. Manual Data Entry Errors
In traditional systems, healthcare providers often rely on manual data entry, which is prone to human error. These errors can occur in patient details, diagnosis codes, and billing information, leading to incorrect claims submissions. A single mistake can result in claim rejections or denials, causing delays in payment and additional administrative work to correct the issue.
2. Slow Claims Processing
Claim submission and processing can take days, even weeks, when handled manually. With a large volume of claims to manage, it’s easy for errors and delays to occur, leading to slow reimbursements. The longer claims take to process, the longer healthcare providers have to wait for their revenue, which can directly affect cash flow.
3. Inefficient Denial Management
One of the most time-consuming challenges in traditional RCM is managing denials. Denied claims require immediate action to resolve, but without an automated system to track and analyze these denials, healthcare providers risk losing significant revenue. Manual tracking often results in missed denials or slow responses, which can hurt overall revenue collection.
4. Complex Compliance Management
The healthcare industry is heavily regulated, with ever-changing policies and compliance requirements. Traditional RCM in medical billing often struggles to keep up with these changes manually. Providers must continuously ensure their billing processes meet regulatory standards, which can be cumbersome and lead to compliance issues, fines, or penalties if not managed correctly.
5. Lack of Real-Time Insights
Traditional RCM systems provide limited or no access to real-time data, which is crucial for identifying and addressing problems before they affect the revenue cycle. Without access to accurate, up-to-date information, healthcare providers are unable to make informed decisions about billing and revenue collection, leading to missed opportunities for optimizing financial outcomes.
These challenges can result in significant revenue losses, reduced efficiency, and increased overhead costs for healthcare providers. Adopting automation in RCM processes is the key to overcoming these hurdles and improving revenue cycle performance.
Why Automation in RCM is Essential
Automation is no longer just a trend; it’s a necessity for healthcare providers seeking to optimize their RCM in medical billing. The following reasons highlight the importance of automation in transforming the revenue cycle management process:
1. Improves Accuracy and Reduces Errors
Manual billing processes are prone to human errors, from data entry mistakes to incorrect coding. Automation eliminates these risks by ensuring accurate, consistent, and error-free claim submissions. By reducing mistakes in revenue cycle management solutions, healthcare providers can prevent costly denials, avoid rework, and significantly improve their revenue integrity.
This leads to faster reimbursements and less administrative burden, allowing healthcare organizations to focus on patient care instead of billing issues.
2. Speeds Up the Billing Process
Time is money, especially in healthcare. Automation accelerates the RCM cycle in medical billing by automating tasks such as claim submission, payment posting, and billing statement generation. This results in faster claim processing, quicker payments, and more efficient financial operations.
By streamlining these processes, automation helps healthcare providers improve cash flow and reduce the time it takes to receive payments from insurers or patients.
3. Enhances Compliance and Regulatory Adherence
Healthcare regulations are complex and frequently updated. Manual processes can struggle to keep pace with these changes, putting healthcare organizations at risk of non-compliance and penalties. Automation ensures that RCM in medical billing is always aligned with the latest regulations, payer policies, and billing codes.
Automated systems can continuously monitor and update processes, ensuring that healthcare providers remain compliant, reduce audit risks, and stay ahead of industry standards.
By integrating automation into revenue cycle management solutions, healthcare providers can address these critical challenges, improve operational efficiency, and ultimately drive better financial performance.
How Automation Is Improving Important Areas of RCM
Automation is revolutionizing key areas of RCM in medical billing, leading to enhanced efficiency, improved accuracy, and faster revenue recovery. Below are the significant areas where automation is making a substantial impact:
1. Claims Management and Submission
Automated claims management systems streamline the process of submitting, tracking, and managing claims. By automating claim creation and submission, healthcare providers can reduce the chance of human error, ensuring more accurate claims.
- Statistic: Automated claims submission reduces claim rejection rates by up to 40% compared to manual processes.
- Automated systems can also verify patient data in real time, ensuring that claims are submitted with correct patient details, codes, and required documents, significantly reducing claim denials.
2. Payment Posting and Reconciliation
Manually posting payments and reconciling accounts can take hours or even days. Automation eliminates these delays by automatically posting payments from both insurance companies and patients, updating patient balances, and reconciling accounts with minimal intervention.
- Statistic: Healthcare organizations that implemented automated payment posting have seen a 25% improvement in cash flow within the first year of implementation.
- By automating payment posting, providers can ensure that patient balances are updated in real-time, reducing delays and improving accuracy.
3. Denial Management and Resolution
Denial management is one of the most tedious and time-consuming aspects of RCM in medical billing. Automated denial management systems can quickly identify and categorize denied claims, allowing staff to prioritize resolution based on denial reason and amount.
- Statistic: Automation in denial management can reduce denial rates by up to 20% and improve resolution times by 30%.
- Automation also provides actionable insights into the root causes of denials, enabling healthcare providers to address recurring issues and improve future claim submissions.
4. Patient Billing and Statements
Automated systems generate accurate, timely patient bills, ensuring that patients are invoiced correctly and on time. These systems can also send automated reminders and notifications, reducing late payments and improving the overall patient experience.
- Statistic: Automation in patient billing can reduce payment delays by up to 40%, improving overall revenue collection.
- Patients benefit from clearer, more detailed billing statements, and automated reminders ensure timely payments, contributing to better cash flow for healthcare providers.
5. Analytics and Reporting
Automated analytics and reporting tools provide real-time insights into the entire RCM cycle in medical billing. Healthcare providers can track key performance indicators (KPIs), identify bottlenecks, and gain insights into financial performance, all of which are critical for optimizing revenue cycle operations.
- Statistic: Healthcare organizations that leverage automated reporting tools have seen a 35% improvement in operational efficiency and decision-making.
- These tools can also predict cash flow trends, identify areas for improvement, and ensure that key financial metrics are met on time.
By automating critical areas of revenue cycle management solutions, healthcare providers can reduce manual workloads, minimize errors, and ultimately improve financial performance.
The Future Trends of Automation in RCM
The future of RCM in medical billing is driven by innovative automation trends that will enhance efficiency and accuracy. Here are three key trends to watch:
1. AI and Machine Learning for Predictive Analytics
AI and machine learning will enable predictive analytics, allowing healthcare providers to foresee claim denials or payment delays before they occur, leading to proactive interventions.
- Benefit: Increased claim approval rates and reduced billing errors.
- Statistic: AI-powered analytics can improve claim approval rates by 20% and reduce billing errors by 30%.
2. Robotic Process Automation (RPA) for Routine Tasks
RPA will automate repetitive tasks like data entry and claim submission, reducing manual work and improving operational efficiency.
- Benefit: Faster claims processing and reduced administrative costs.
- Statistic: RPA adoption in RCM can reduce administrative costs by up to 40%.
3. Blockchain for Secure Billing and Payments
Blockchain will enhance billing security by providing transparent, tamper-proof transaction records, reducing fraud, and improving payment reconciliation.
- Benefit: Increased security and transparency in financial transactions.
- Statistic: Blockchain can reduce fraud by up to 50% and improve reconciliation times.
These trends signal a future where automation in RCM enhances both financial and operational outcomes for healthcare organizations.
Final Words
Digital transformation is essential for improving efficiency in healthcare, especially when it comes to RCM in medical billing. Helixbeat offers solutions that make billing processes faster, more accurate, and efficient. With advanced tools like PULSE and FUSION, they use AI and cloud technology to give real-time insights and keep patient data secure.
Helixbeat’s digital transformation services help healthcare organizations tackle challenges and improve their operations. If you’re looking to improve your RCM cycle in medical billing, Helixbeat can help. Contact us today to see how their services can make your business run more smoothly and efficiently.
FAQ
1. What is RCM in medical billing, and why is it important?
RCM (Revenue Cycle Management) in medical billing refers to the process of managing the financial aspects of patient care, from initial scheduling and registration to final payment. It’s important because it ensures timely payments, reduces errors, and improves cash flow for healthcare providers.
2. How does automation improve the RCM process?
Automation in RCM helps reduce manual errors, speeds up claims processing, and ensures accurate billing. It also provides real-time updates, improves denial management, and accelerates reimbursement, ultimately increasing efficiency and revenue.
3. What are the benefits of using AI in RCM?
AI enhances RCM by predicting claim denials, identifying errors early, and optimizing the billing process. It allows for faster and more accurate claim submissions, reducing the chances of errors and rejections, which helps improve overall financial performance.
4. How can blockchain impact RCM in medical billing?
Blockchain technology provides secure and transparent billing systems, reducing fraud and ensuring that all transactions are recorded accurately. It also helps streamline the payment process and improve trust between healthcare providers and payers.
5. What challenges do healthcare organizations face with traditional RCM systems?
Traditional RCM systems often involve manual processes, which are prone to errors, delays, and inefficiencies. These systems can lead to claim rejections, delayed payments, and higher operational costs, ultimately affecting revenue and patient satisfaction.